We get sent for an EDP (emotionally disturbed person). The cop meets us outside and says it is an old lady with Alzheimers. She took the trash out in her nightgown even though the trash doesn't get picked up today. This has happened before -- the woman wandering the neighborhood in her nightgown. Her husband came out to get her and she attacked him, scratching him quite viciously. She is now saying the neighbors attacked the house with snowballs and beat her husband up. The cop says the husband can't handle her anymore.
We go inside and find a sweet old woman sitting in her nightgown in an arm chair in the living room.
"I don't want to go to the hospital," she says.
"You brought this on. You brought this all on yourself," the husband says.
Another police office tries to usher the husband back into the kitchen.
"But they attacked our house," she says. "The neighbors."
"In your dreams," the husband shouts. "In your dreams!"
"Will my husband be coming to the hospital with me?" the woman asks me.
"No," he shouts again. "Take her out with the trash for all I care!"
***
In the ambulance, I ask her questions to test her memory. She is able to answer some, but not others.
She thinks today is Christmas. She knows her birthday. She says she thinks they have lived in their house for twenty years.
I ask her how old she was when she met her husband. She says she was twenty-five, but she doesn't remember where she met him.
They had a big wedding. They are Greek. Niether of them were good dancers.
She doesn't remember the names of her children. They are grown up and married.
She doesn't know what happened today or why she is in the ambulance.
"What qualities did your husband have that made you want to marry him?" I ask.
She thinks a moment, then smiles, remembering. "He is a kind man," she says. "Always very considerate. Courteous. He always treats me well."
This paramedic blog contains notes from my journal. Some of the characters, details, dates and settings have been changed to protect the confidentiality of people and patients involved.
Saturday, December 31, 2005
Thursday, December 29, 2005
Pastry
The call is for severe bleeding. It turns out to be a burst abscess in a teenage male, who three weeks ago tore his hamstring. He bled internally , but the blood wasn't reabsorbed by the body and an abscess started to grow. He was scheduled to have surgery to remove the undrained blood. At first I didn't know what it was. His friend was holding pressure on it, and had told me about spurting blood. We removed the pressure and then after a moment's delay this huge bloblike hunk of blood began to flow out of the large open wound. I covered it right back up and held pressure. He screamed. When I uncovered it at the hospital for the doctor, I saw it was just pus. It was like pus from a boil, except it was at first, dark red, then pinky, almost pepperminty in color. The pus that flowed out just kept coming. It didn't stop.
I go down to the nurse's station to give my report to the nurse. He hasn't seen the patient yet. As I am giving my report the nurse is chowing down on these little pastries. He hands me a creme-filled one. I stare at it a moment, then back at the nurse. Then as soon as I am done with my report, I walk around the corner and drop the pastry in the trash can.
"I'm going down to the cafeteria," my partner says. "You coming?"
"I'll eat later," I say.
I go down to the nurse's station to give my report to the nurse. He hasn't seen the patient yet. As I am giving my report the nurse is chowing down on these little pastries. He hands me a creme-filled one. I stare at it a moment, then back at the nurse. Then as soon as I am done with my report, I walk around the corner and drop the pastry in the trash can.
"I'm going down to the cafeteria," my partner says. "You coming?"
"I'll eat later," I say.
Sunday, December 25, 2005
Christmas
Last night I watched Scrooged, the Bill Murray version of a Christmas Carrol, where Murray is the bah humbug head of a big TV network. Bill Murray is a very funny actor, and Scrooged always chokes me up at the end, when the little mute kid speaks for the first time and says "God Bless us Everyone." Then they all start singing "Put a Little Love in Your Heart" with Murray singing like his old Saturday Night Live lounge singer character.
Sometimes I feel like I am a Scrooge. I am always working on Christmas. My brother invited me to go to New Jersey and have Christmas with him and his family this year. Of course I couldn't go -- I had to work.
What kind of a bah humbug am I? Working on Christmas all the time. But working in EMS on Christmas is different than working a regular job on Christmas. I have always been proud that when my name is written in the book, I can be counted on to be there. It is not like we can just close up shop on Christmas. Christmas falls on my day to work, I work it. I like being reliable.
I read an interesting article -- "Will Words Fail Her?" -- about a young Chinese fiction writer, Yiyun Li, who wrote a great collection of short stories called A Thousand Years of Good Prayers. One of her teachers, James Alan McPherson, who was also a teacher of mine many years ago, was quoted in the article as saying in American fiction, we have lost the community voice. It is all about the self, but that community voice still exists in writers in Japan and China, writers like Li.
One of her teachers, James Alan McPherson, who was also a teacher of mine many years ago, was quoted in the article as saying in American fiction, we have lost the community voice. It is all about the self, but that community voice still exists in writers in Japan and China, writers like Li.
In this job over time you can lose yourself. You become a part of the community, the blanket of watchfulless over the cities and towns that you cover, and that becomes more important than who you are as an individual. People say it is bad to lose yourself in your job, and I don't disagree -- you need balance in your own life. But at the same time, I don't think it is neccessarily all bad.
In Scrooged, Murray's ex-boss, who comes back as the dead Jacob Marley, says his work, his life should have been that of mankind, not TV ratings. While I am not knocking the fact that today I am getting paid double time and a half holiday pay, I think you can make the arguement that our work in EMS is not the work of material advancement, but the work of mankind. There is a certain privledge in looking out over the community, in being its protector, particularly on Christmas Day.
There are some sacrifices in this job, and I am not advocating putting it before everything else in your life, but if you find meaning, even redemption in your work, that is no small thing.
Sometimes I feel like I am a Scrooge. I am always working on Christmas. My brother invited me to go to New Jersey and have Christmas with him and his family this year. Of course I couldn't go -- I had to work.
What kind of a bah humbug am I? Working on Christmas all the time. But working in EMS on Christmas is different than working a regular job on Christmas. I have always been proud that when my name is written in the book, I can be counted on to be there. It is not like we can just close up shop on Christmas. Christmas falls on my day to work, I work it. I like being reliable.
I read an interesting article -- "Will Words Fail Her?" -- about a young Chinese fiction writer, Yiyun Li, who wrote a great collection of short stories called A Thousand Years of Good Prayers.
In this job over time you can lose yourself. You become a part of the community, the blanket of watchfulless over the cities and towns that you cover, and that becomes more important than who you are as an individual. People say it is bad to lose yourself in your job, and I don't disagree -- you need balance in your own life. But at the same time, I don't think it is neccessarily all bad.
In Scrooged, Murray's ex-boss, who comes back as the dead Jacob Marley, says his work, his life should have been that of mankind, not TV ratings. While I am not knocking the fact that today I am getting paid double time and a half holiday pay, I think you can make the arguement that our work in EMS is not the work of material advancement, but the work of mankind. There is a certain privledge in looking out over the community, in being its protector, particularly on Christmas Day.
There are some sacrifices in this job, and I am not advocating putting it before everything else in your life, but if you find meaning, even redemption in your work, that is no small thing.
Saturday, December 24, 2005
Imagine
I rarely follow up with my patients. If they are in the ED when I come back with a new patient, I will stop in and see how thay are doing. Or I might ask a nurse or a doctor what was the deal with a certain recent patient from earlier in the day or maybe even the day before, but I am not one of these guys who is always going up to the floors to reintroduce myself to the patient as the paramedic who brought them in. Not that there is anything wrong with it. I did it a few times when I first started. Haven't for years.
A couple weeks ago, we did a code save. I wrote about it in an entry titled Blanket. It was my third code save this year. By "save" I am using the iffy terminology of a cardiac arrest patient brought to the ED with a blood pressure and still alive when we left the ED.
When it comes to cardiac arrests, unless they are talking to me when I leave the ER, I guess I just assume they die eventually. I was surprised once. I got called for a stroke. I found a man sitting on a neighbor's garbadge can, where he had been talking to them after driving up in his car, when he suddenly slumped over. We went lights and sirens to the hospital following the stoke protocol. I dug his ID out of his wallet and was shocked by the name. It was the same name as a man I had done in a cardiac arrest a year before. I'd gotten a pressure back, but never thought anything more of it. I just assumed he had died or was a vegetable in some nursing home. To make it an even better story, his massive stroke turned out to be a TIA and he was talking to me before we even reached the hospital. He was in fact the same guy. At the hospital I met his family and they said they had tried to get in contact with me. They had gone to the fire station to leave a message for me, but hadn't heard anything back. Niether had I. That day in the ER at our little reunion we all shook hands and hugged, and smiled a lot.
With that story in mind, and because on this code -- as I have written before, my two partners were a young man going through the EMT class and a two decades of experience plus EMT, both of whom it was their first code save -- I thought it would be nice to find out how the lady was doing. She was after all breathing on her own on the way in. I had found out that a week later she was still alive in the ICU although I had no report on her condition.
I began to imagine her alive. I imagined us visiting her back in her home with her family and all her granchildren and great grandchildren around her. I thought how happy my partners would feel. For one it would be the crowning achievement of his career, for the other, an indelible moment that would guide him toward a long rewarding lifetime in EMS.
I went in to see the hospital's EMS coordinator and ask him if he could look up the three code saves I had this year, particularly the last one, to see how they made out. He said it would take some leg work, but he would be happy to do it for me.
I thanked him, then went out to the car, and just happened to open up the newspaper. There she was on the obituary page. Our "save." A 93-year old great great grandmother. Died in the hospital. Rest in peace. I saw the coordinator later that day and thanked him for his offer, but told him not to bother looking up the others.
A couple weeks ago, we did a code save. I wrote about it in an entry titled Blanket. It was my third code save this year. By "save" I am using the iffy terminology of a cardiac arrest patient brought to the ED with a blood pressure and still alive when we left the ED.
When it comes to cardiac arrests, unless they are talking to me when I leave the ER, I guess I just assume they die eventually. I was surprised once. I got called for a stroke. I found a man sitting on a neighbor's garbadge can, where he had been talking to them after driving up in his car, when he suddenly slumped over. We went lights and sirens to the hospital following the stoke protocol. I dug his ID out of his wallet and was shocked by the name. It was the same name as a man I had done in a cardiac arrest a year before. I'd gotten a pressure back, but never thought anything more of it. I just assumed he had died or was a vegetable in some nursing home. To make it an even better story, his massive stroke turned out to be a TIA and he was talking to me before we even reached the hospital. He was in fact the same guy. At the hospital I met his family and they said they had tried to get in contact with me. They had gone to the fire station to leave a message for me, but hadn't heard anything back. Niether had I. That day in the ER at our little reunion we all shook hands and hugged, and smiled a lot.
With that story in mind, and because on this code -- as I have written before, my two partners were a young man going through the EMT class and a two decades of experience plus EMT, both of whom it was their first code save -- I thought it would be nice to find out how the lady was doing. She was after all breathing on her own on the way in. I had found out that a week later she was still alive in the ICU although I had no report on her condition.
I began to imagine her alive. I imagined us visiting her back in her home with her family and all her granchildren and great grandchildren around her. I thought how happy my partners would feel. For one it would be the crowning achievement of his career, for the other, an indelible moment that would guide him toward a long rewarding lifetime in EMS.
I went in to see the hospital's EMS coordinator and ask him if he could look up the three code saves I had this year, particularly the last one, to see how they made out. He said it would take some leg work, but he would be happy to do it for me.
I thanked him, then went out to the car, and just happened to open up the newspaper. There she was on the obituary page. Our "save." A 93-year old great great grandmother. Died in the hospital. Rest in peace. I saw the coordinator later that day and thanked him for his offer, but told him not to bother looking up the others.
Friday, December 23, 2005
Alone
A sixty year old woman who lives alone feels her throat begining to swell. This is not the first time it has happened -- she has a history of angioedema -- so she knows what to do. She takes her closest epi-pen (She has ten scattered about the house) and injects herself with the lifesaving drug, and then calls 911.
She is still having some trouble swallowing when we get there. "It's getting easier," she says. "Thank you for coming so quickly."
I listen to her throat. There is a good flow of air.
She is sitting on the short steps that lead from the living room up to the second level of the house. "I was scared there for a moment," she says. She is a short, squat greyhaired woman, who speaks very deliberately. "It's been quite a week for me. I didn't need this."
"What hospital do you want to go to?"
"This is not how I wanted to spend the night." She sounds like she has the weight of the world on her shoulders.
"Someone has to let the dogs in," she says. "They can't be left outside. They're too old."
I offer to do it, even though I hate dogs. I open up the back door, and say, here, pouchies, then I hear some chains rattling and the rustle of two big dogs approaching and then I see they are German Shepards. I have had some terrible experiences with German Shepards in my life -- one taking a bite out of my butt when I was riding my bike as a five year old, and then another dog -- Stormy -- terrorizing me in the neighborhood when I was in junior high. But these dogs are nice, and give me no trouble and come right in and approach their owner who gives them hugs and tells them to be good, while she puts some water in their dishes.
On the way in to the hospital, the woman tells me she had just been diagnosed with cancer and is scheduled for surgery in January. "I'm going to have to put them down."
"They seem okay."
Her voice quivers. "No, they are old and incontinent and there will be no one to take care of them when I'm sick. With the surgery, and then the chemo, and the radiation, I don't want to put them through that."
"Don't you have family in the area? Someone to look after them."
She shakes her head. "No, it's just me."
"That's too bad."
"They've lived good lives."
"I guess maybe being put down isn't the worst way to go. In this job, you come to feel good for people who die in their sleep."
She breaks into a smile, as she looks almost inward. "You can't get much better than to die in the arms of someone who loves you."
And then there is silence between us.
She cries quietly.
She is still having some trouble swallowing when we get there. "It's getting easier," she says. "Thank you for coming so quickly."
I listen to her throat. There is a good flow of air.
She is sitting on the short steps that lead from the living room up to the second level of the house. "I was scared there for a moment," she says. She is a short, squat greyhaired woman, who speaks very deliberately. "It's been quite a week for me. I didn't need this."
"What hospital do you want to go to?"
"This is not how I wanted to spend the night." She sounds like she has the weight of the world on her shoulders.
"Someone has to let the dogs in," she says. "They can't be left outside. They're too old."
I offer to do it, even though I hate dogs. I open up the back door, and say, here, pouchies, then I hear some chains rattling and the rustle of two big dogs approaching and then I see they are German Shepards. I have had some terrible experiences with German Shepards in my life -- one taking a bite out of my butt when I was riding my bike as a five year old, and then another dog -- Stormy -- terrorizing me in the neighborhood when I was in junior high. But these dogs are nice, and give me no trouble and come right in and approach their owner who gives them hugs and tells them to be good, while she puts some water in their dishes.
On the way in to the hospital, the woman tells me she had just been diagnosed with cancer and is scheduled for surgery in January. "I'm going to have to put them down."
"They seem okay."
Her voice quivers. "No, they are old and incontinent and there will be no one to take care of them when I'm sick. With the surgery, and then the chemo, and the radiation, I don't want to put them through that."
"Don't you have family in the area? Someone to look after them."
She shakes her head. "No, it's just me."
"That's too bad."
"They've lived good lives."
"I guess maybe being put down isn't the worst way to go. In this job, you come to feel good for people who die in their sleep."
She breaks into a smile, as she looks almost inward. "You can't get much better than to die in the arms of someone who loves you."
And then there is silence between us.
She cries quietly.
Sunday, December 18, 2005
Diamond in the Rough (Update)
Back in August I posted the first three chapters of a novel I have been revising called Diamond in the Rough. Instead of posting additional chapters on this site, I have set up a secondary site where the chapters can be read by those interested. I will post on here when I have added new chapters. Right now I have chapters 1-9 posted.
Before you read them and pass judgement, I need to add some cautions and qualifiers. There are characters in this book (particuarly Fred) who do things that I do not obviously endorse. My main character (the narrator), who I hope will be viewed as symphathetic, will do things that are clearly unacceptable. This novel is based on a true incident, and grew out of a challenge I gave myself to find out why someone did what they did, and to try to write a story that might explain how someone would come to do such a deed. While some people may take offense to the behavior of some EMTs in this story, as they should, I hope in the end that the book will offer some kind of redemption. Lastly while the book is based on a true incident, all of the characters are entirely fictional. Any resemblence to real people is entirely coincidental.
Here then is the link:
Diamond in the Rough
Before you read them and pass judgement, I need to add some cautions and qualifiers. There are characters in this book (particuarly Fred) who do things that I do not obviously endorse. My main character (the narrator), who I hope will be viewed as symphathetic, will do things that are clearly unacceptable. This novel is based on a true incident, and grew out of a challenge I gave myself to find out why someone did what they did, and to try to write a story that might explain how someone would come to do such a deed. While some people may take offense to the behavior of some EMTs in this story, as they should, I hope in the end that the book will offer some kind of redemption. Lastly while the book is based on a true incident, all of the characters are entirely fictional. Any resemblence to real people is entirely coincidental.
Here then is the link:
Diamond in the Rough
Sunday, December 11, 2005
A Blanket
It is during the tail end of a snow storm that has left ten inches in six hours. We are on the way back from the hospital after a call where we had to wade through deep drifts to get to a patient's farmhouse. The roads are barely plowed. We get called for a 93-year old woman unresponsive with shallow breathing. Updated to respirations at six a minute, now irregular and gasping. I say it's going to be a code. When we get there instead of trying to haul the stretcher through the snow, we grab the equipment and go right in. We have to walk through a narrow hallway, through an open living room, then down some stairs to the basement, then down another corridor and into a small bedroom where a man and younger woman stand, and there on the bed is an old woman who from the door I could see is not breathing.
I'm thinking great, 93 years old not breathing. She is dead. Has the family even thought about what they want us to do? I say (I really do say) "Have you thought at all about what you would like us to do if she stops breathing or her heart stops and she dies." I feel for a pulse. There is none. "Like now. Would you like us to resuscitate her?"
The man seems understandably flustered by my question, and hesitates and then says something to the effect of well, yes, yes we do.
"It's a code," I tell my partner who has followed me down the narrow hallway and into the bedroom. "Let's get her on the floor." We pick her up and place her on the floor so there is room for one person at the head and room between the end of the bed and the dresser for someone to do compressions. I hand one partner the ambu bag, then the other partner -- an EMT student, the young ex-high school football player, who has been doing so well riding with us -- I tell to do compressions, (Let's do the new CPR, I say, 30 and 2) while I get the defib pads out, hook them up to the monitor, then slap them on. I have them stop for a moment, and I quickly see the woman is asystole.
I tell them to continue and not stop, while I get out my intubation kit. I also hand an oral airway to my partner, and tell him to take out her false teeth. The bottom teeth come out, but the top, he says are nailed in.
I take out a number 8 tube. I see the epiglottis, see the chords, have a little trouble getting the tube to go into the chords, as the lady's teeth stick up and there is not a lot of room between the blade, the teeth and the side's of her mouth. I reshape the tube, making it straighter and I am able to easily pass it. The bulb syringe test works. No sound in the belly. Equal and strong on the right and left. Vapor in the tube. I tie it up with the commercial holder. I hand it over to my partner and say, keep it in there. Squeeze the bag 8 times a minute.
Then, instead of dropping some epi down the tube like I always do, I delay and go for an IV. As I am pulling out my IV kit I remember I need to attach the capnography. I attach the capnography device between the tube and the bag and then into the machine. I glance at the reading. It says 35. I am shocked. 35 is normal. It is also an excellent prognosticator. On the other hand the lady looks dead and is asystole.
I get a 20 in the AC. I have them stop CPR. Still asystole, then I tell them to resume. I take out a milligram of epi and say, "All right, let's see if the epi can do it's job," and I slam the epi followed by an atropine.
I look up at the monitor and see a funky rhythm.
Shock or not shock. I hold off because it looks organized.
I give another epi. We continue CPR. The young man is doing deep strong compressions. We're bagging nice and slowly.
When we stop again, it looks like there is a qrs complex, then some loopy ventricular like rolls, then a qrs.
I go so far as to hit the charge button, but I hold off.
There is a rhythm trying to break in.
And there it is.
No question about it.
"Check for pulses," I say.
"Strong radial pulse," my partner says. "Very rapid."
I look at the monitor. A Sinus tack at 132 that over the next several minutes gradually comes down to the low 100s.
93 years old and we get her back -- at least temporarily. As we package her up, I stay vigilant waiting for the epi to wear off, but she's hanging right in there. Good rhythm, good end tidal. Good BP.
We have a difficult extrication. We can't get the stretcher in the house. We have to strap her to the board, securing her head with head blocks. A police officer and I carry her down the hall stopping every ten seconds or so to ventilate her. The stair is a bitch. We have to pass her up nearly vertical. Her family waits in the living room. Suddenly they are yelling at us. "Put a sheet on her." "You can't take her out like that." "Let me get a blanket." "Have some respect for her modesty."
I am doing my best to keep her from toppling off the board. I hadn't even thought about her exposed breasts. I was concerned with just getting her to the ambulance. They are yelling at me. It occurs to me then that they have no idea about her condition. I normally try to involve the family, and keep them updated, but due to the geography of the scene, I was isolated from them. I remember what I read in Thom Dick's book, People Care: Career-Friendly Practices for Professional Caregivers. .
.
"People don't remember much about our medicine. But they do remember how we make them feel."-Thom Dick
We have no sheets handy. Our stretcher is outside in the snow. I set her down because I don't want to drop her and it's time for more ventilation.
"She'll be cold," a family member says.
I want to explain what I have just read in the new AHA guidelines about the benefits of hypothermia and how keeping her from getting too hot is good for her. "Her situation is very critical," I say. "We need to get her to the ambulance." I glance at the monitor. Still holding her own. "We'll get her covered up." I nod to the officer to pick her up again.
Normally, on a code I always pause, and have the family say something to the patient, even though she may not be able to hear. I do it for the family to let them at least have a chance to say goodbye because most of the time the patient is dead by the time they arrive. But I am not even thinking about that now. I'm just thinking about getting her out to the ambulance through the snow before she loses her pulse.
We back out the door, and down the icy steps, and out to where to the stretcher is set up. There we bag her again, and throw a blanket on her. In the back of the ambulance, we switch her to the main 02, and head to the hospital. Everything status quo. The EMT student is bagging. I compliment him on how well he has done on the call, but I tell him we can't expect the woman to ever walk out of the hospital. At her age and given the condition we found her in, it just isn't going to happen. He nods and says nothing.
A moment later the woman moves suddenly. It startles both of us. And then we see her chest heave again. And again. And to my amazement she is breathing on her own.
"But then again," I say. "I could be wrong."
At the hospital, her pressure is 130/60. Her heart rate is 104. Her respiratory rate is 10.
The doctor congratulates us and I praise my crew. My regular partner has worked EMS as a volunteer for 20 years and this is his first save. The EMT student has just begun his career. I am still startled that we got back a 93 year old woman from asystole. She had to have stopped breathing just minutes before our arrival. I tried to use the new AHA guidelines. Good CPR, less ventilations. No drugs down the tube. Even unconsciously hypothermia. And while the AHA guidelines say our cardiac drugs have never been proven to help. I know she responded to the epi. I have seen it before. Epi IV has gotten me back many an arrested patient, or at least gotten them to the hospital alive.
But before I congratulate myself too much, after I have written the run form and dropped it off with the nurse, I glance at the patient's room and see two family members sitting in armless chairs by her side. Their eyes meet mine. They stare at me but give no expression. I feel like they are waiting for me to say something.
I approach, and bow my head slightly. They remain seated. "I am sorry about not covering her up," I say. I should have gotten a blanket."
"That's all right," the woman says. "Thank you."
"I wanted to get her out to the ambulance. I wasn't thinking."
"Thank you," she says. "Thank you for helping."
I bow my head slightly again, and then head back down the hall.
Lesson learned.
I'm thinking great, 93 years old not breathing. She is dead. Has the family even thought about what they want us to do? I say (I really do say) "Have you thought at all about what you would like us to do if she stops breathing or her heart stops and she dies." I feel for a pulse. There is none. "Like now. Would you like us to resuscitate her?"
The man seems understandably flustered by my question, and hesitates and then says something to the effect of well, yes, yes we do.
"It's a code," I tell my partner who has followed me down the narrow hallway and into the bedroom. "Let's get her on the floor." We pick her up and place her on the floor so there is room for one person at the head and room between the end of the bed and the dresser for someone to do compressions. I hand one partner the ambu bag, then the other partner -- an EMT student, the young ex-high school football player, who has been doing so well riding with us -- I tell to do compressions, (Let's do the new CPR, I say, 30 and 2) while I get the defib pads out, hook them up to the monitor, then slap them on. I have them stop for a moment, and I quickly see the woman is asystole.
I tell them to continue and not stop, while I get out my intubation kit. I also hand an oral airway to my partner, and tell him to take out her false teeth. The bottom teeth come out, but the top, he says are nailed in.
I take out a number 8 tube. I see the epiglottis, see the chords, have a little trouble getting the tube to go into the chords, as the lady's teeth stick up and there is not a lot of room between the blade, the teeth and the side's of her mouth. I reshape the tube, making it straighter and I am able to easily pass it. The bulb syringe test works. No sound in the belly. Equal and strong on the right and left. Vapor in the tube. I tie it up with the commercial holder. I hand it over to my partner and say, keep it in there. Squeeze the bag 8 times a minute.
Then, instead of dropping some epi down the tube like I always do, I delay and go for an IV. As I am pulling out my IV kit I remember I need to attach the capnography. I attach the capnography device between the tube and the bag and then into the machine. I glance at the reading. It says 35. I am shocked. 35 is normal. It is also an excellent prognosticator. On the other hand the lady looks dead and is asystole.
I get a 20 in the AC. I have them stop CPR. Still asystole, then I tell them to resume. I take out a milligram of epi and say, "All right, let's see if the epi can do it's job," and I slam the epi followed by an atropine.
I look up at the monitor and see a funky rhythm.
Shock or not shock. I hold off because it looks organized.
I give another epi. We continue CPR. The young man is doing deep strong compressions. We're bagging nice and slowly.
When we stop again, it looks like there is a qrs complex, then some loopy ventricular like rolls, then a qrs.
I go so far as to hit the charge button, but I hold off.
There is a rhythm trying to break in.
And there it is.
No question about it.
"Check for pulses," I say.
"Strong radial pulse," my partner says. "Very rapid."
I look at the monitor. A Sinus tack at 132 that over the next several minutes gradually comes down to the low 100s.
93 years old and we get her back -- at least temporarily. As we package her up, I stay vigilant waiting for the epi to wear off, but she's hanging right in there. Good rhythm, good end tidal. Good BP.
We have a difficult extrication. We can't get the stretcher in the house. We have to strap her to the board, securing her head with head blocks. A police officer and I carry her down the hall stopping every ten seconds or so to ventilate her. The stair is a bitch. We have to pass her up nearly vertical. Her family waits in the living room. Suddenly they are yelling at us. "Put a sheet on her." "You can't take her out like that." "Let me get a blanket." "Have some respect for her modesty."
I am doing my best to keep her from toppling off the board. I hadn't even thought about her exposed breasts. I was concerned with just getting her to the ambulance. They are yelling at me. It occurs to me then that they have no idea about her condition. I normally try to involve the family, and keep them updated, but due to the geography of the scene, I was isolated from them. I remember what I read in Thom Dick's book, People Care: Career-Friendly Practices for Professional Caregivers.
"People don't remember much about our medicine. But they do remember how we make them feel."-Thom Dick
We have no sheets handy. Our stretcher is outside in the snow. I set her down because I don't want to drop her and it's time for more ventilation.
"She'll be cold," a family member says.
I want to explain what I have just read in the new AHA guidelines about the benefits of hypothermia and how keeping her from getting too hot is good for her. "Her situation is very critical," I say. "We need to get her to the ambulance." I glance at the monitor. Still holding her own. "We'll get her covered up." I nod to the officer to pick her up again.
Normally, on a code I always pause, and have the family say something to the patient, even though she may not be able to hear. I do it for the family to let them at least have a chance to say goodbye because most of the time the patient is dead by the time they arrive. But I am not even thinking about that now. I'm just thinking about getting her out to the ambulance through the snow before she loses her pulse.
We back out the door, and down the icy steps, and out to where to the stretcher is set up. There we bag her again, and throw a blanket on her. In the back of the ambulance, we switch her to the main 02, and head to the hospital. Everything status quo. The EMT student is bagging. I compliment him on how well he has done on the call, but I tell him we can't expect the woman to ever walk out of the hospital. At her age and given the condition we found her in, it just isn't going to happen. He nods and says nothing.
A moment later the woman moves suddenly. It startles both of us. And then we see her chest heave again. And again. And to my amazement she is breathing on her own.
"But then again," I say. "I could be wrong."
At the hospital, her pressure is 130/60. Her heart rate is 104. Her respiratory rate is 10.
The doctor congratulates us and I praise my crew. My regular partner has worked EMS as a volunteer for 20 years and this is his first save. The EMT student has just begun his career. I am still startled that we got back a 93 year old woman from asystole. She had to have stopped breathing just minutes before our arrival. I tried to use the new AHA guidelines. Good CPR, less ventilations. No drugs down the tube. Even unconsciously hypothermia. And while the AHA guidelines say our cardiac drugs have never been proven to help. I know she responded to the epi. I have seen it before. Epi IV has gotten me back many an arrested patient, or at least gotten them to the hospital alive.
But before I congratulate myself too much, after I have written the run form and dropped it off with the nurse, I glance at the patient's room and see two family members sitting in armless chairs by her side. Their eyes meet mine. They stare at me but give no expression. I feel like they are waiting for me to say something.
I approach, and bow my head slightly. They remain seated. "I am sorry about not covering her up," I say. I should have gotten a blanket."
"That's all right," the woman says. "Thank you."
"I wanted to get her out to the ambulance. I wasn't thinking."
"Thank you," she says. "Thank you for helping."
I bow my head slightly again, and then head back down the hall.
Lesson learned.
Friday, December 09, 2005
People Care
If you are looking to get someone in EMS a great Christmas present, here is the book for them or for yourself:
People Care: Career-Friendly Practices for Professional Caregivers
Thom Dick is the author of Street Talk , a book of essays that came out about the time I was in EMT school in 1989. It was extremely influential in instructing me in what it meant to be a caregiver. It encouraged me to see the patient as a person, to respect the people I work with, to take the time to be kind, and other important lessons that helped me become a better EMT.
, a book of essays that came out about the time I was in EMT school in 1989. It was extremely influential in instructing me in what it meant to be a caregiver. It encouraged me to see the patient as a person, to respect the people I work with, to take the time to be kind, and other important lessons that helped me become a better EMT.
A few years later I heard him speak at an EMS convention and he was fantastic. He got you fired up to go out there and hold old ladies' hands. He made you feel like the work you did, even the mundane parts, was special. I read his book often over the years and it always charged me up. Now I don't pretend to have always lived up to his standards. I know I haven't. But I do try.
His new book seems to be a expansion/complilation of his prior book and the talks he gives all over the country. It is enhanced by cartoons by Steve Berry, who does the I am Not an Ambulance Driver cartoon series.
"When you kneel in front of somebody's granpa who's sitting on his couch and denying his chest pain, you need to recognize the pain he says isn't there, detect the shortness of breath he hasn't mentioned and sense the fear that's absolutely dominating his conciousness. You need to appreciate the fact that his spouse, seated right there next to him, is scared to death she's never going to sleep with him again. And somehow, you need to make everything better in just a few minutes.
These are the dynamics of even the simplest emergency response. They presuppose the presence of gifts in us that not even the greatest teacher can impart -- gifts that unfortunately, come without instructions.
This book is an examination of those gifts and a collection of the instructions that didn't come with them. It's based on the collective experience and wisdom of dozens of professional paramedics and EMTs worlwide who learned to love the lifelong pursuit of helping others.
We hope it helps you to join their number."
- from back cover of book
"People don't remember much about our medicine. But they do remember how we make them feel."
-Thom Dick
"It's not enough to be the most competent EMT you can be. You need to be nice. And it's not enough to be nice. You need to be competent and nice."
-Thom Dick
People Care: Career-Friendly Practices for Professional Caregivers
Thom Dick is the author of Street Talk
A few years later I heard him speak at an EMS convention and he was fantastic. He got you fired up to go out there and hold old ladies' hands. He made you feel like the work you did, even the mundane parts, was special. I read his book often over the years and it always charged me up. Now I don't pretend to have always lived up to his standards. I know I haven't. But I do try.
His new book seems to be a expansion/complilation of his prior book and the talks he gives all over the country. It is enhanced by cartoons by Steve Berry, who does the I am Not an Ambulance Driver cartoon series.
"When you kneel in front of somebody's granpa who's sitting on his couch and denying his chest pain, you need to recognize the pain he says isn't there, detect the shortness of breath he hasn't mentioned and sense the fear that's absolutely dominating his conciousness. You need to appreciate the fact that his spouse, seated right there next to him, is scared to death she's never going to sleep with him again. And somehow, you need to make everything better in just a few minutes.
These are the dynamics of even the simplest emergency response. They presuppose the presence of gifts in us that not even the greatest teacher can impart -- gifts that unfortunately, come without instructions.
This book is an examination of those gifts and a collection of the instructions that didn't come with them. It's based on the collective experience and wisdom of dozens of professional paramedics and EMTs worlwide who learned to love the lifelong pursuit of helping others.
We hope it helps you to join their number."
- from back cover of book
"People don't remember much about our medicine. But they do remember how we make them feel."
-Thom Dick
"It's not enough to be the most competent EMT you can be. You need to be nice. And it's not enough to be nice. You need to be competent and nice."
-Thom Dick
Thursday, December 08, 2005
New AHA CPR and ECG Guidelines
I'm like a kid before Christmas waiting for the new AHA CPR and ECC guidelines to come out. For almost a year I have been following the evidence sheets posted on the Heart Association web site, and nearly everyday in November checked the site for the new guidelines to be posted. When they finally came out over a week ago, I downloaded them and have been pouring over them. The guidelines are exciting to me because they represent the synthesis of expert's opinions after reviewing all the studies of the last five years, they give a glimpse of how EMS will be in the near future and they are full of instructive PEARLS. (Reading them line by line is an excellent educational learning experience. My copy of the 2000 guidelines is heavily highlighted and dog-eared.) Also, as someone involved in writing my region's protocols, I am interested in how they may have to be rewritten.
There are some interesting changes in the new guidelines, some of which have already made the news:
Cardiac Arrest:
CPR for lay people is now 30 compressions to 2 respirations for adults instead of 15:2.
When EMS response to a cardiac arrest is 4-5 minutes or when EMS responders did not witness the arrest, EMS providers may do 2 minutes of CPR prior to defibrillation.
1 shock instead of 3 stacked: Rescuers should resume CPR immediately after shocking and continue for 2 minutes before checking for pulse or to shock again. Rescuers should continue CPR during the charging phase of defib until time to clear.
The first shock should be 360 monophasic or 150-200 for biphasic.
The focus is on compressions. "Simply put: rescuers should push hard, push fast, allow full chest recoil, minimize interruptions in compressions, and defibrillate promptly when appropriate."
Ventilations should be 8 to 10 per minute in the intubated patient in arrest; 10 to 12 with a perfusing rhytmn.
Pacing for asystole is no longer recommended.
Unless special siuations are present (hypothermia)"cessation of efforts in the out-of-hospital setting, following system-specific criteria and under direct medical control, should be standard practice in all EMS systems."
Cardiac arrest associated with Trauma
If intubation is performed in the field, it should be done during transport.
Volume infusion for trauma is recommended only for patients with isolated head or extremity trauma with goal of systolic >100.
Tachycardias
Lidociane is no longer in the algorithm for tachycardia with pulses. It's amiodarone.
Rapid afib has new language that says "we recommend expert consultation if the patient is stable." The phrase runs throughout the section. "Stable patients may await expert consultation because treatment has the potential for harm."
ACS
Nitro has new restrictions in the setting of ACS. No nitro for heart rates less than 50 and more than 100. And no nitro if the BP is 30 mm Hg below patient's baseline, rather than just below 90 mm Hg.
Asthma
Steroids should be administered to all asthma patients as early as possible.
Anaphylaxis
Epi 1:1000 should be administered IM not SQ.
***
I am anxious to discuss the new guidelines at our MAC meeting next week and hear other people's opinions.
Much of it makes sense to me. The focus on compressions I think is huge. As I have written before I have been on many scenes where CPR just doesn't get done. Someone's going for the tube, someone's going for the IV, someones getting the board and no one is on compressions. And it seems everytime I come upon a code where only first responders are there, all I hear is the defib unit going, "checking pulses, if no pulses..." and everyone just standing there. When compressions do get done, they are often done poorly. When I started really focusing on compressions, my save rate (at least rate to the hospital with pulses) went up considerably.
I worry a little about the ventilations not getting done. I also worry about people getting shocked as they want compressions to continue even when the defib is charging. Still I'm for the changes. What we have right now isn't working very well. Hopefully this will be better.
From a medic standpoint I was a little discouraged that I got a bit of an anti-medic feeling reading the guidelines. Now let me say, I believe these guidelines are pro-patient, and anything pro-patient has to also be pro-medic because medics are for what is best for the patient. What I mean is that so much that medics do seems to be being discredited -- and maybe for the best. From fluid rescusitation for trauma, to intubation(the text is full of caution about the pitfalls of intubation), to the curious language of seeking "expert consultation," the message seems to be just take them to the hospital without harming them. You can't argue with "Do No Harm" if it is harm that we have been doing.
On the other hand, there is full recognition that if we can't bring someone back in the field, they will not be brought back in the ED. (It is time to end futile resuscitations and senseless transports of dead people.)
I believe in and trust experts, I just hope however that there were medics or at least pro-medic people at the table to see that the evidence was interpreted in a way that wasn't biased against what we do, or interpreted with a proper understanding of what and how we do what we do.
Lastly, I must say just because the meds we give during codes haven't been proven to work doesn't mean medics aren't worth anything. It means the meds aren't worth anything. I believe medics are very important, but they are only as good as their education, their training, their oversight, and the equipment, meds, and tools they are given to do the job.
***
Major Changes in the 2005 AHA Guidelines for CPR and ECC. Reaching the Tipping Point for Change
And a link to all the abstracts:
Circulation Selected Abstracts
***
Added 12/11/05
There are three publications that can be downloaded:
View the C2005 International Consensus on CPR and ECC Science with Treatment Recommendations
View the 2005 AHA Guidelines for CPR and ECC
Currents 2005 Highlights
Eventually, I'm guessing in the spring, the AHA will be selling paperbound copies of the guidlines and science as they have done in the past.
There are some interesting changes in the new guidelines, some of which have already made the news:
Cardiac Arrest:
CPR for lay people is now 30 compressions to 2 respirations for adults instead of 15:2.
When EMS response to a cardiac arrest is 4-5 minutes or when EMS responders did not witness the arrest, EMS providers may do 2 minutes of CPR prior to defibrillation.
1 shock instead of 3 stacked: Rescuers should resume CPR immediately after shocking and continue for 2 minutes before checking for pulse or to shock again. Rescuers should continue CPR during the charging phase of defib until time to clear.
The first shock should be 360 monophasic or 150-200 for biphasic.
The focus is on compressions. "Simply put: rescuers should push hard, push fast, allow full chest recoil, minimize interruptions in compressions, and defibrillate promptly when appropriate."
Ventilations should be 8 to 10 per minute in the intubated patient in arrest; 10 to 12 with a perfusing rhytmn.
Pacing for asystole is no longer recommended.
Unless special siuations are present (hypothermia)"cessation of efforts in the out-of-hospital setting, following system-specific criteria and under direct medical control, should be standard practice in all EMS systems."
Cardiac arrest associated with Trauma
If intubation is performed in the field, it should be done during transport.
Volume infusion for trauma is recommended only for patients with isolated head or extremity trauma with goal of systolic >100.
Tachycardias
Lidociane is no longer in the algorithm for tachycardia with pulses. It's amiodarone.
Rapid afib has new language that says "we recommend expert consultation if the patient is stable." The phrase runs throughout the section. "Stable patients may await expert consultation because treatment has the potential for harm."
ACS
Nitro has new restrictions in the setting of ACS. No nitro for heart rates less than 50 and more than 100. And no nitro if the BP is 30 mm Hg below patient's baseline, rather than just below 90 mm Hg.
Asthma
Steroids should be administered to all asthma patients as early as possible.
Anaphylaxis
Epi 1:1000 should be administered IM not SQ.
***
I am anxious to discuss the new guidelines at our MAC meeting next week and hear other people's opinions.
Much of it makes sense to me. The focus on compressions I think is huge. As I have written before I have been on many scenes where CPR just doesn't get done. Someone's going for the tube, someone's going for the IV, someones getting the board and no one is on compressions. And it seems everytime I come upon a code where only first responders are there, all I hear is the defib unit going, "checking pulses, if no pulses..." and everyone just standing there. When compressions do get done, they are often done poorly. When I started really focusing on compressions, my save rate (at least rate to the hospital with pulses) went up considerably.
I worry a little about the ventilations not getting done. I also worry about people getting shocked as they want compressions to continue even when the defib is charging. Still I'm for the changes. What we have right now isn't working very well. Hopefully this will be better.
From a medic standpoint I was a little discouraged that I got a bit of an anti-medic feeling reading the guidelines. Now let me say, I believe these guidelines are pro-patient, and anything pro-patient has to also be pro-medic because medics are for what is best for the patient. What I mean is that so much that medics do seems to be being discredited -- and maybe for the best. From fluid rescusitation for trauma, to intubation(the text is full of caution about the pitfalls of intubation), to the curious language of seeking "expert consultation," the message seems to be just take them to the hospital without harming them. You can't argue with "Do No Harm" if it is harm that we have been doing.
On the other hand, there is full recognition that if we can't bring someone back in the field, they will not be brought back in the ED. (It is time to end futile resuscitations and senseless transports of dead people.)
I believe in and trust experts, I just hope however that there were medics or at least pro-medic people at the table to see that the evidence was interpreted in a way that wasn't biased against what we do, or interpreted with a proper understanding of what and how we do what we do.
Lastly, I must say just because the meds we give during codes haven't been proven to work doesn't mean medics aren't worth anything. It means the meds aren't worth anything. I believe medics are very important, but they are only as good as their education, their training, their oversight, and the equipment, meds, and tools they are given to do the job.
***
Major Changes in the 2005 AHA Guidelines for CPR and ECC. Reaching the Tipping Point for Change
And a link to all the abstracts:
Circulation Selected Abstracts
***
Added 12/11/05
There are three publications that can be downloaded:
View the C2005 International Consensus on CPR and ECC Science with Treatment Recommendations
View the 2005 AHA Guidelines for CPR and ECC
Currents 2005 Highlights
Eventually, I'm guessing in the spring, the AHA will be selling paperbound copies of the guidlines and science as they have done in the past.
Monday, December 05, 2005
Bathroom Break
Today I did something for the first time I had never ever done before while working in EMS. In this job you learn when you are sitting around waiting for a call that if the urge to use the bathroom comes upon you, you act on it because it sucks to be suddenly hurtling down the road on your way to a cardiac arrest having thinking to yourself, "Boy do I have to pee. Damn, I should have peed when I had the urge." Or worse. Once you get on the call, however, your adrenaline takes over and your urge fades to the background at least until you get to the hospital, then as soon as you have unloaded your patient and turned over care, you make a beeline to the bathroom.
Here's what happened today. We get called for "leg pain" and climb the stairs of an apartment to the second floor to find a large(220 plus) 50-year old woman sitting on the bedspread of a kingsize bed on top of a bed pan, with her pajama pants pulled down. Her aged mother says the patient, her daughter, hasn't gotten out of bed for five days even though there is nothing wrong with her. She has a history of mental illness but has not been on any medications or seen any doctors for over a year. She refuses to get out of bed for us. I ask the patient why she can't get out of bed, she says her leg is stiff, but when we approach, she seems to be moving it very well when she tries to kick us. Her mother says she is also diabetic, so to check her sugar, it takes three of us to hold her down while she kicks and tries to swing her arms and bite us. Her sugar is 148 -- normal.
We discuss our options then with the police officer. I say it is clear she is a threat to herself. She is obviously mentally ill. He questions her some and agrees. We each take a turn trying to persuade her that she needs to come with us, but she will have none of it. Even our threat to remove her by force doesn't phase her. "Bring it on," she says, "I ain't going."
We are on the second floor and stairwell is narrow. None of us is looking forward to wrestling with her, and fighting with her down the stairs. We decide to try to just medicate her. I tell everyone that once I give her the medicine we will need to wait at least ten minutes for it to take effect. A few weeks ago, I sedated a 16-year old in the city and the cops were impatient and tried to move her before the medicine had a chance to really work so she fought us, kicking and screaming all the way out to the ambulance, and only then after we had tied her down did she fall asleep.
The cop starts writing a PEER(Police Emergency Evaluation Request) that gives us the power to take her against her will. I prepare my two syringes. As I lay out my equipment -- the narc kit which has the ativan, the med kit which has the haldol, the IV kit that has the syringes and alcohol -- I think that I should have a premade sedation kit (like the OB kits), but one that would include a tape of relaxation music -- the sound of waves or light rainfall -- to put on the music player and maybe candles or incense to burn. When I am ready, the others hold her down, while I wipe her arm down then inject her, first with the Ativan, then with the haldol. Then we sit back and wait.
Suddenly I have a terrible stomach ache. I try to ignore it, but it only worsens. I have had stomach aches before on the job, but then I was always caught up in the call and managed to fight through it. But here I am standing waiting -- at least ten minutes for the drugs to take effect -- and I am about fifteen feet from the patient's open bathroom door. I try to suck it in, but it is like a stabbing knife. I think about my ability to keep it in if the medicine maybe doesn't work that well -- the patient is a big woman, and we have to carry her fighting down the stairs. Finally I can't take it anymore. I ask the patient's mother if I may use the bathroom. She says yes, and a few minutes later, I walk back out. Are you okay? they ask. I nodd. Just fine, thank you. I am a new man.
We wait another five minutes, and then pick the woman up with minimal resistance, place her on the stair chair, carry her down to the stretcher, and she sleeps all the way to the hospital.
Here's what happened today. We get called for "leg pain" and climb the stairs of an apartment to the second floor to find a large(220 plus) 50-year old woman sitting on the bedspread of a kingsize bed on top of a bed pan, with her pajama pants pulled down. Her aged mother says the patient, her daughter, hasn't gotten out of bed for five days even though there is nothing wrong with her. She has a history of mental illness but has not been on any medications or seen any doctors for over a year. She refuses to get out of bed for us. I ask the patient why she can't get out of bed, she says her leg is stiff, but when we approach, she seems to be moving it very well when she tries to kick us. Her mother says she is also diabetic, so to check her sugar, it takes three of us to hold her down while she kicks and tries to swing her arms and bite us. Her sugar is 148 -- normal.
We discuss our options then with the police officer. I say it is clear she is a threat to herself. She is obviously mentally ill. He questions her some and agrees. We each take a turn trying to persuade her that she needs to come with us, but she will have none of it. Even our threat to remove her by force doesn't phase her. "Bring it on," she says, "I ain't going."
We are on the second floor and stairwell is narrow. None of us is looking forward to wrestling with her, and fighting with her down the stairs. We decide to try to just medicate her. I tell everyone that once I give her the medicine we will need to wait at least ten minutes for it to take effect. A few weeks ago, I sedated a 16-year old in the city and the cops were impatient and tried to move her before the medicine had a chance to really work so she fought us, kicking and screaming all the way out to the ambulance, and only then after we had tied her down did she fall asleep.
The cop starts writing a PEER(Police Emergency Evaluation Request) that gives us the power to take her against her will. I prepare my two syringes. As I lay out my equipment -- the narc kit which has the ativan, the med kit which has the haldol, the IV kit that has the syringes and alcohol -- I think that I should have a premade sedation kit (like the OB kits), but one that would include a tape of relaxation music -- the sound of waves or light rainfall -- to put on the music player and maybe candles or incense to burn. When I am ready, the others hold her down, while I wipe her arm down then inject her, first with the Ativan, then with the haldol. Then we sit back and wait.
Suddenly I have a terrible stomach ache. I try to ignore it, but it only worsens. I have had stomach aches before on the job, but then I was always caught up in the call and managed to fight through it. But here I am standing waiting -- at least ten minutes for the drugs to take effect -- and I am about fifteen feet from the patient's open bathroom door. I try to suck it in, but it is like a stabbing knife. I think about my ability to keep it in if the medicine maybe doesn't work that well -- the patient is a big woman, and we have to carry her fighting down the stairs. Finally I can't take it anymore. I ask the patient's mother if I may use the bathroom. She says yes, and a few minutes later, I walk back out. Are you okay? they ask. I nodd. Just fine, thank you. I am a new man.
We wait another five minutes, and then pick the woman up with minimal resistance, place her on the stair chair, carry her down to the stretcher, and she sleeps all the way to the hospital.
Sunday, December 04, 2005
Scandanavian Beauty
We get a third party call for a woman with abdominal pain coughing up blood. The neighbor meets us at the door and tells us the older woman is feeling woozy, and has been coughing up bright red blood. She also mentions that she hasn't been acting quite right. Yesterday she was out raking the other neighbor's yard instead of her own.
As we walk through the old farmhouse, which is immaculately kept with beautiful hardwood floors and antique furniture. I begin to remember being in this house before. And once I see the old woman in her upstairs bedroom, it all comes back to me. Several years ago we were called to this same house because no one would answer the phone and the woman who lived here hadn't been seen for awhile. We pounded on the door. No answer. We finally broke in and walked quickly through the rooms of the house looking for someone on the ground with a broken hip, someone stroked out, or maybe someone cold rigored and stiff. The cop and I walked right through the bedroom and into the large bathroom, then turned around and came back through the bedroom and there she was sitting in a big velvet backed arm chair by her bed, completely naked, looking like she had just gotten out of a sauna, watching us without saying a word, off in her own world, a cup of hot tea in her hands. She was in her eighties, but all I can say is she was a Scandanavian beauty with a chest that Raquel Welch would have been proud of. Tonight she is sitting in the same chair, except she has a bathrobe on and her skin is jaundiced, and she looks frail and much older. The clean carpet is scattered with tissues tinged with blood. She still has her tea and we let her finish drinking it before we carry her down in the stair chair.
As we walk through the old farmhouse, which is immaculately kept with beautiful hardwood floors and antique furniture. I begin to remember being in this house before. And once I see the old woman in her upstairs bedroom, it all comes back to me. Several years ago we were called to this same house because no one would answer the phone and the woman who lived here hadn't been seen for awhile. We pounded on the door. No answer. We finally broke in and walked quickly through the rooms of the house looking for someone on the ground with a broken hip, someone stroked out, or maybe someone cold rigored and stiff. The cop and I walked right through the bedroom and into the large bathroom, then turned around and came back through the bedroom and there she was sitting in a big velvet backed arm chair by her bed, completely naked, looking like she had just gotten out of a sauna, watching us without saying a word, off in her own world, a cup of hot tea in her hands. She was in her eighties, but all I can say is she was a Scandanavian beauty with a chest that Raquel Welch would have been proud of. Tonight she is sitting in the same chair, except she has a bathrobe on and her skin is jaundiced, and she looks frail and much older. The clean carpet is scattered with tissues tinged with blood. She still has her tea and we let her finish drinking it before we carry her down in the stair chair.
Thursday, December 01, 2005
Apnea
On another site I keep a daily journal. I record evey call I do in a day along with some observations. It is from this journal that I draw most of the material for this blog. Here I try to write simple stories that I have given some thought too. There I just write whatever I think of when I get home. Some days its pretty boring, some its repetitive. Because of the nature of confidentiality, I don't use my name on that site because it identifies the calls as date specific, and even though I may change many of the details, I just prefer to leave it more anynomous. Reviewing what I have written over the last year, shows too many days when all I am writing about is a broken EMS system. Here is part of a recent entry(I did rewrite it some. I can't help myself).
A 97 year-old-man whith a poor gait falls twice in his apartment in a residential community. He is not hurt, but according to the nurse he is not as spry as he used to be(like when he was 96) and hasn't been eating as much and, fall once, you get a free pass, fall twice, it's a trip to the hospital. We go to a distant hospital because that's where his doctor is based, not that his doctor is going to come in and see him on a Sunday.
A nursing home calls a commercial service to transport a patient not as responsive as usual, which usually isn't much. The commercial call-taker hears the word "unresponsive" and passes(as directed by state mandate) the call to us -- the local 911 provider. Because it is now a 911 call, our police dispatcher sends two police cars lights and sirens, in addition to us, who are coming from the distant hospital. The cops skid into the curb, run inside and find no nurses or aides. They find a patient "not breathing" and put her on oxygen and she immediately starts breathing. They finally find a nurse and what develops is a heated arguement about elder abuse, complete with "I want your name" and "I want your name."
That's when we come in. Now I have often been to this nursing home and found patients in dire straights with no nurses anywhere to be found to give me a report, and the nurse who is here today is one of the worst offenders, but when I enter the room, the patient seems fine. She does have periods of apnea, but I have taken her in before and that is normal for her. Sometimes she just isn't as perky in her semi-responsive way as she is on better days. The patient has every diagnosis possible: CVA, Dementia, diaylsis, MI, CHF, NIDDM, Alzheimers, HTN, Seizure, etc. And of course she is a full code. I guess the officers came in during one of the apnea periods. They thought she wasn't breathing, they put her on an 02 mask and whalla, she started breathing.
The officers should never have been sent in the first place. It was after all just a nursing home "emergifer(emergency transfer/unscheduled transfer)." And of course they were never told it was an commercial pass. They thought they were responding to a life and death emergency. They found a patient "not breathing" unattended by a nurse or even a nurse's aide. From where they are coming from, they were rightly upset. But to the nurse it was just a transfer and she had other patients to attend to because the truth is nursing homes are notoriously understaffed.
I love being a medic and like working on the regional EMS committees. But somedays I wish I was in charge of the whole shebang with unlimited power, then I could fix some of these things. Fix the apnea in the system.
A 97 year-old-man whith a poor gait falls twice in his apartment in a residential community. He is not hurt, but according to the nurse he is not as spry as he used to be(like when he was 96) and hasn't been eating as much and, fall once, you get a free pass, fall twice, it's a trip to the hospital. We go to a distant hospital because that's where his doctor is based, not that his doctor is going to come in and see him on a Sunday.
A nursing home calls a commercial service to transport a patient not as responsive as usual, which usually isn't much. The commercial call-taker hears the word "unresponsive" and passes(as directed by state mandate) the call to us -- the local 911 provider. Because it is now a 911 call, our police dispatcher sends two police cars lights and sirens, in addition to us, who are coming from the distant hospital. The cops skid into the curb, run inside and find no nurses or aides. They find a patient "not breathing" and put her on oxygen and she immediately starts breathing. They finally find a nurse and what develops is a heated arguement about elder abuse, complete with "I want your name" and "I want your name."
That's when we come in. Now I have often been to this nursing home and found patients in dire straights with no nurses anywhere to be found to give me a report, and the nurse who is here today is one of the worst offenders, but when I enter the room, the patient seems fine. She does have periods of apnea, but I have taken her in before and that is normal for her. Sometimes she just isn't as perky in her semi-responsive way as she is on better days. The patient has every diagnosis possible: CVA, Dementia, diaylsis, MI, CHF, NIDDM, Alzheimers, HTN, Seizure, etc. And of course she is a full code. I guess the officers came in during one of the apnea periods. They thought she wasn't breathing, they put her on an 02 mask and whalla, she started breathing.
The officers should never have been sent in the first place. It was after all just a nursing home "emergifer(emergency transfer/unscheduled transfer)." And of course they were never told it was an commercial pass. They thought they were responding to a life and death emergency. They found a patient "not breathing" unattended by a nurse or even a nurse's aide. From where they are coming from, they were rightly upset. But to the nurse it was just a transfer and she had other patients to attend to because the truth is nursing homes are notoriously understaffed.
I love being a medic and like working on the regional EMS committees. But somedays I wish I was in charge of the whole shebang with unlimited power, then I could fix some of these things. Fix the apnea in the system.
Sunday, November 27, 2005
Kind of Friends
We get called for an OD. A young woman took all her psych meds at the same time because she was depressed. Her ex-boyfriend broke into her house and stole her cell phone. And her best female friend committed suicide recently, so she was just feeling a little overwhelmed. She had a past history of suicide attempts, but she said she wasn't try to hurt herself this time -- she just wanted to chill out. Sitting in a chair in the kitchen she was slurring her speech, and when she tried to stand, her balance was poor. At first I thought she was in her late thirties. I found out she was just thirty.
We got her out in the ambulance and she lay down on the stretcher, and despite the wear and tear on her face, I could see she was actually a fairly pretty girl. It didn't hurt that she was wearing a tank top that showed off a decent body -- one that she said she used to spend a lot of time in the gymn toning -- lifting weights, doing cardio. She had a flat abdomen with a navel ring, and a chest that certainly would have had the guys in the gymn checking her out when she walked past. She had beautiful long hair.
I told her I had to do an IV and when I looked at her arms, I could see track marks. "Good luck," she said. "My veins suck. When I used to work out they were bulging ropes. Not any more."
"Where do they sometimes find a vein?" I asked.
"Between my toes."
No, she didn't actually say that. She said, as she turned her wrist at a peculiar angle, and then with her mouth, kissed the inside aspect, "Right about here, if you wap it a couple times, a little one might pop up."
I couldn't find anything there. Instead I found a vein I could put a 24 in in her forearm. It was hidden from view, but I could feel it beneath the surface with my finger tips. I sunk it and filled four blood tubes.
"You're good," she said.
I was impressed with myself. I was thinking maybe she'll invite me to shoot her and her pals up at their next house party. But...
When we were talking about working out and why she hadn't been in the gymn, she said she stopped going after she got burned. She'd had to go to rehab instead. She told me how her ex-roommate -- a woman she'd met in N.A. -- a woman who she said was "kind of paranoid" -- had poured boiling water on her one night when she was sleeping, and said, "You're not so pretty now, are you dearie?" For a couple years after that she could barely lift her arm above her shoulder, although it was better now.
Not the kind of friends I would want to hang around with. It was amazing she wasn't scared more badly. You could see the burns on her neck, but her face with the help of grafts and a damn good surgeon, made her look okay considering.
Hard life.
We got her out in the ambulance and she lay down on the stretcher, and despite the wear and tear on her face, I could see she was actually a fairly pretty girl. It didn't hurt that she was wearing a tank top that showed off a decent body -- one that she said she used to spend a lot of time in the gymn toning -- lifting weights, doing cardio. She had a flat abdomen with a navel ring, and a chest that certainly would have had the guys in the gymn checking her out when she walked past. She had beautiful long hair.
I told her I had to do an IV and when I looked at her arms, I could see track marks. "Good luck," she said. "My veins suck. When I used to work out they were bulging ropes. Not any more."
"Where do they sometimes find a vein?" I asked.
"Between my toes."
No, she didn't actually say that. She said, as she turned her wrist at a peculiar angle, and then with her mouth, kissed the inside aspect, "Right about here, if you wap it a couple times, a little one might pop up."
I couldn't find anything there. Instead I found a vein I could put a 24 in in her forearm. It was hidden from view, but I could feel it beneath the surface with my finger tips. I sunk it and filled four blood tubes.
"You're good," she said.
I was impressed with myself. I was thinking maybe she'll invite me to shoot her and her pals up at their next house party. But...
When we were talking about working out and why she hadn't been in the gymn, she said she stopped going after she got burned. She'd had to go to rehab instead. She told me how her ex-roommate -- a woman she'd met in N.A. -- a woman who she said was "kind of paranoid" -- had poured boiling water on her one night when she was sleeping, and said, "You're not so pretty now, are you dearie?" For a couple years after that she could barely lift her arm above her shoulder, although it was better now.
Not the kind of friends I would want to hang around with. It was amazing she wasn't scared more badly. You could see the burns on her neck, but her face with the help of grafts and a damn good surgeon, made her look okay considering.
Hard life.
Thursday, November 24, 2005
Thanksgiving
It’s Thanksgiving morning. I awake at 5:10, shower and dress, then open up the garage door to see a couple inches of snow on the ground. It’s beautiful, but I hate winter, hate the cold weather, hate driving in snow.
When I get to the base, I can see from the tracks in the snow by the ambulance doors. The night crew is out on a call. Ten minutes later I hear them clear with a presumption. I sit in the office and drink a diet coke while I read the morning paper.
This week a thirty-year-old female cop in one of the suburban towns was murdered by her ex-boyfriend, a state cop. We had two cars on standby while they looked for the shooter. They found him a couple hours later, also dead. The paper said he parked his car at a park, and then walked over to her house so she wouldn’t see him. He lay in wait for her and when she returned from work, he ambushed her, shooting her three times, twice in the chest and once in the head. He was supposed to turn himself into court today on a police charge, but instead he called his lawyer and said there was a change in plans. The lawyer got the message a couple hours later and alerted police. Her new boyfriend -- another cop -- came home and found her.
I knew her by face, not by name. I’d been on calls with her a few times over the six years. I remember when she first started working. She was gorgeous. It was hard to believe someone that good-looking would chose to be a cop. Lately I noticed she’d started to wear a bit more makeup around her eyes, her face seemed a little heavier. She never had much to say to us, at least on the calls I went on. She was all business. If she pulled you over, I don't think you'd want to sweet talk her. I’m sure she had a warm side she showed to those who knew her.
The paper in the news rack the next day had a headline “A Cop’s Fury.” It had pictures of the two dead on the front. It made me think, you are here one day, and the next people are walking by the news rack with your picture on it, only you aren’t one of the people walking by to see it.
**
We did a call in her town this morning, and said our condolences to the two cops who were there. They had black bands over their badges. The call was for an old woman who said she had taken a handful of painkillers. She said she did it because she was stupid. She said her ex-husband and her doctor would be mad. I got the feeling from the cops they were at this house all the time for similar vague complaints of taking too many pills. “I don’t need this today,” one cop said to me.
**
All week I have found myself in idle moments thinking about the dead policewoman. I guess she probably never figured her death was coming that day. She comes home from work, sits down with computer and then suddenly there is the angry man in her house, gun drawn coming at it. Did she know she was going to die?
When do heart attack victims get that sense that right now what is happening -- this sudden pain in their chest -- might be their end? And car crash victims – they start to loose control and see the tree or the truck careening toward them?
Last New Year’s Eve another cop in the same department was gunned down at a domestic. I knew him too, but also just in passing. We’d been on calls together. A nice, big friendly man. He walked down the basement stairs and then shooter pulled the trigger on a machine gun. Did he have time to realize his end had come?
This summer a paramedic student who rode with me was on a jet ski with his girl friend in Florida when they were blindsided by a boat. I heard about it when I saw his obituary posted at the office. Did he hear the roar of the engine? Did he turn to see it bearing down on him? What did he think in those moments?
Last Saturday they held a memorial for a flight nurse who died in a helicopter crash 13 years ago. I was working in the health department at the time and remember the late night call I got telling me about the crash. I’d seen her around the ER a few times when I brought in patients as a volunteer EMT. And I had ridden in the helicopter as a third rider only a month before. The accident happened when the copter clipped a wire while trying to land near a highway rest stop, a rest stop that now bears her name. When the copter started spinning, did she know?
I don’t mean to be morbid.
The saddest thing about all these deaths is not just the fear they must have felt when they saw what was happening to them, but that fact that everything that would have happened in their lives and all the people they would have affected is just gone. The children the might have had, the things those children would have gone on to do, the memories – all of it vanished. That’s the tragedy.
Death happens everyday and we see it in this job, but it doesn’t impact as much unless it is one of us. You can grow immune to it until it comes close like it has again this week.
But I don’t worry as much about dying as I used to. I’ve lived awhile now and feel lucky to have made it as long as I have. If the deal was when I was born, I agreed to come out of the womb, but in return I would only have these 47 years, I'd take that deal anytime.
I have many, many years ahead I hope. But if I were to die today, if the door were to open and death were to be there, I would be terrified, but I can’t say that I would have been cheated. Life, with its share of sadness and disappointments, has been largely good to me. And today I am as excited about life and its possibilities as I ever have been, excited not in the wild way I was as a youth, but in the more realistic sense that I can enjoy the moments now and not just the thought of the goal.
I want to live fully and feel, for the most part, I have been. I work a lot, but I like my job and the money I make will help me keep doing what I love – being a paramedic, writing, going to foreign countries to help the poor, getting good seats to a Red Sox game every year, living in my house which I feel comfortable in, being able to eat a good steak, and drink a cold beer when I want without having to count nickels on the liquor store counter.
I have much to be thankful for today.
I hope I continue to live a full life and that the door doesn’t open for me any time soon.
Please not any time soon.
I don't want my picture on the news rack, my obit posted on some bulletin board, people thinking, yeah, I knew that guy. We did a few calls together. I used to see him around.
When I get to the base, I can see from the tracks in the snow by the ambulance doors. The night crew is out on a call. Ten minutes later I hear them clear with a presumption. I sit in the office and drink a diet coke while I read the morning paper.
This week a thirty-year-old female cop in one of the suburban towns was murdered by her ex-boyfriend, a state cop. We had two cars on standby while they looked for the shooter. They found him a couple hours later, also dead. The paper said he parked his car at a park, and then walked over to her house so she wouldn’t see him. He lay in wait for her and when she returned from work, he ambushed her, shooting her three times, twice in the chest and once in the head. He was supposed to turn himself into court today on a police charge, but instead he called his lawyer and said there was a change in plans. The lawyer got the message a couple hours later and alerted police. Her new boyfriend -- another cop -- came home and found her.
I knew her by face, not by name. I’d been on calls with her a few times over the six years. I remember when she first started working. She was gorgeous. It was hard to believe someone that good-looking would chose to be a cop. Lately I noticed she’d started to wear a bit more makeup around her eyes, her face seemed a little heavier. She never had much to say to us, at least on the calls I went on. She was all business. If she pulled you over, I don't think you'd want to sweet talk her. I’m sure she had a warm side she showed to those who knew her.
The paper in the news rack the next day had a headline “A Cop’s Fury.” It had pictures of the two dead on the front. It made me think, you are here one day, and the next people are walking by the news rack with your picture on it, only you aren’t one of the people walking by to see it.
**
We did a call in her town this morning, and said our condolences to the two cops who were there. They had black bands over their badges. The call was for an old woman who said she had taken a handful of painkillers. She said she did it because she was stupid. She said her ex-husband and her doctor would be mad. I got the feeling from the cops they were at this house all the time for similar vague complaints of taking too many pills. “I don’t need this today,” one cop said to me.
**
All week I have found myself in idle moments thinking about the dead policewoman. I guess she probably never figured her death was coming that day. She comes home from work, sits down with computer and then suddenly there is the angry man in her house, gun drawn coming at it. Did she know she was going to die?
When do heart attack victims get that sense that right now what is happening -- this sudden pain in their chest -- might be their end? And car crash victims – they start to loose control and see the tree or the truck careening toward them?
Last New Year’s Eve another cop in the same department was gunned down at a domestic. I knew him too, but also just in passing. We’d been on calls together. A nice, big friendly man. He walked down the basement stairs and then shooter pulled the trigger on a machine gun. Did he have time to realize his end had come?
This summer a paramedic student who rode with me was on a jet ski with his girl friend in Florida when they were blindsided by a boat. I heard about it when I saw his obituary posted at the office. Did he hear the roar of the engine? Did he turn to see it bearing down on him? What did he think in those moments?
Last Saturday they held a memorial for a flight nurse who died in a helicopter crash 13 years ago. I was working in the health department at the time and remember the late night call I got telling me about the crash. I’d seen her around the ER a few times when I brought in patients as a volunteer EMT. And I had ridden in the helicopter as a third rider only a month before. The accident happened when the copter clipped a wire while trying to land near a highway rest stop, a rest stop that now bears her name. When the copter started spinning, did she know?
I don’t mean to be morbid.
The saddest thing about all these deaths is not just the fear they must have felt when they saw what was happening to them, but that fact that everything that would have happened in their lives and all the people they would have affected is just gone. The children the might have had, the things those children would have gone on to do, the memories – all of it vanished. That’s the tragedy.
Death happens everyday and we see it in this job, but it doesn’t impact as much unless it is one of us. You can grow immune to it until it comes close like it has again this week.
But I don’t worry as much about dying as I used to. I’ve lived awhile now and feel lucky to have made it as long as I have. If the deal was when I was born, I agreed to come out of the womb, but in return I would only have these 47 years, I'd take that deal anytime.
I have many, many years ahead I hope. But if I were to die today, if the door were to open and death were to be there, I would be terrified, but I can’t say that I would have been cheated. Life, with its share of sadness and disappointments, has been largely good to me. And today I am as excited about life and its possibilities as I ever have been, excited not in the wild way I was as a youth, but in the more realistic sense that I can enjoy the moments now and not just the thought of the goal.
I want to live fully and feel, for the most part, I have been. I work a lot, but I like my job and the money I make will help me keep doing what I love – being a paramedic, writing, going to foreign countries to help the poor, getting good seats to a Red Sox game every year, living in my house which I feel comfortable in, being able to eat a good steak, and drink a cold beer when I want without having to count nickels on the liquor store counter.
I have much to be thankful for today.
I hope I continue to live a full life and that the door doesn’t open for me any time soon.
Please not any time soon.
I don't want my picture on the news rack, my obit posted on some bulletin board, people thinking, yeah, I knew that guy. We did a few calls together. I used to see him around.
Monday, November 21, 2005
Anonymous-"I'm Human"
The following comment was posted on one of my entries by "anonymous." I thought it was so good, I am reposting it here so those who don't normally read the comments can read it. So to "anonymous" I hope you don't mind my reposting this here. Thank you for your moving account.
Anonymous said...
I struggle with the issues of spirituality. I went on a messy car accident call the other day where some people had been tossed from car that rolled off the road. They were teenagers. One of them was dead right there. Four of the others were transported, and one died a few days later in the hospital.
All five of the occupants, I found out in the newspaper, were close friends. Two were twin brothers. One twin died, the other was the one who died in the hospital. In the space of a week, a mother lost two of her sons.
I live two blocks from where one of the dead twins lived. The church down the street held a prayer vigil for the twin that'd been in the hospital.
Normally, it's pretty anonymous. But this wasn't anonymous enough. I didn't know these people personally, and when I saw the obits, I didn't recognize their picture. In the obit pic, they didn't have blood on their face and vomit in their hair. They didn't have a ET tube in them, or a BVM by their face. They didn't have blood coming out of their ears, or a bone sticking out of their leg. Everyone else remembers them as they lived. I remember them as they died.
I heard people talk about how it was part of God's plan, and how there will be something good that comes out of it.
But to me, it's just shitty luck. They might have been drinking, but no matter what the state police say, it's possible the alcohol wasn't THE factor. Maybe it was changing the radio station at the wrong time, or a tire blowout, or a cell phone call at exactly the wrong time.
I don't know what kind of Plan requires one brother to die in a ditch, and the other to aspirate his stomach contents and die on the vent in the ICU.
I don't see the Good that comes out of something like that. It's shitty luck, that's all. No plan, nothing fantastic. Just another grieving family. All the prayer in the world from all the caring people and pastors didn't help those boys live. They died, but their memories live on in those who didn't. That's the afterlife as I see it.
That call really bothered me for a while. It was one of the first really bad trauma calls I've seen. I'm new, that's why. And that's why it really bothered me.
For two or three days, I kept seeing the mangled bodies around the car. I kept seeing the bloody ambulance floor.
I never once had that whole 'If only I'd..." thing. I know that what we did was flawless. Nothing could save that person. The best I could do was to do my job well enought to, maybe, make it possible for them to die with their family nearby in the hospital.
I'll never forget that call, ever. That moment changed the lives of a lot of people forever. It changed mine too. I learned more about myself and this work and this world in that instant than I ever remember learning before.
In a way, that boy that died lives on in me. He's in my memories. I wish I could say it didn't bother me, but hey, I'm human.
I mention this because your post made me think about the amazing privledge people in EMS have in seeing such unadulerated emotions -- love and hate and terror and joy and fear and relief in such pure forms.
There's precious few times when one can see this in the world, these pure expressions of the human experience.
It is, I think, the best part of EMS -- the honor of being present at so many life changing events. It's not often spoken of in EMS: the honor of bearing witness and filling in the collective memory.
10:41 PM
Anonymous said...
I struggle with the issues of spirituality. I went on a messy car accident call the other day where some people had been tossed from car that rolled off the road. They were teenagers. One of them was dead right there. Four of the others were transported, and one died a few days later in the hospital.
All five of the occupants, I found out in the newspaper, were close friends. Two were twin brothers. One twin died, the other was the one who died in the hospital. In the space of a week, a mother lost two of her sons.
I live two blocks from where one of the dead twins lived. The church down the street held a prayer vigil for the twin that'd been in the hospital.
Normally, it's pretty anonymous. But this wasn't anonymous enough. I didn't know these people personally, and when I saw the obits, I didn't recognize their picture. In the obit pic, they didn't have blood on their face and vomit in their hair. They didn't have a ET tube in them, or a BVM by their face. They didn't have blood coming out of their ears, or a bone sticking out of their leg. Everyone else remembers them as they lived. I remember them as they died.
I heard people talk about how it was part of God's plan, and how there will be something good that comes out of it.
But to me, it's just shitty luck. They might have been drinking, but no matter what the state police say, it's possible the alcohol wasn't THE factor. Maybe it was changing the radio station at the wrong time, or a tire blowout, or a cell phone call at exactly the wrong time.
I don't know what kind of Plan requires one brother to die in a ditch, and the other to aspirate his stomach contents and die on the vent in the ICU.
I don't see the Good that comes out of something like that. It's shitty luck, that's all. No plan, nothing fantastic. Just another grieving family. All the prayer in the world from all the caring people and pastors didn't help those boys live. They died, but their memories live on in those who didn't. That's the afterlife as I see it.
That call really bothered me for a while. It was one of the first really bad trauma calls I've seen. I'm new, that's why. And that's why it really bothered me.
For two or three days, I kept seeing the mangled bodies around the car. I kept seeing the bloody ambulance floor.
I never once had that whole 'If only I'd..." thing. I know that what we did was flawless. Nothing could save that person. The best I could do was to do my job well enought to, maybe, make it possible for them to die with their family nearby in the hospital.
I'll never forget that call, ever. That moment changed the lives of a lot of people forever. It changed mine too. I learned more about myself and this work and this world in that instant than I ever remember learning before.
In a way, that boy that died lives on in me. He's in my memories. I wish I could say it didn't bother me, but hey, I'm human.
I mention this because your post made me think about the amazing privledge people in EMS have in seeing such unadulerated emotions -- love and hate and terror and joy and fear and relief in such pure forms.
There's precious few times when one can see this in the world, these pure expressions of the human experience.
It is, I think, the best part of EMS -- the honor of being present at so many life changing events. It's not often spoken of in EMS: the honor of bearing witness and filling in the collective memory.
10:41 PM
Friday, November 18, 2005
Airway
Did a code at a nursing home last week. Patient, last seen allegedly an hour earlier, found apneic and pulseless in bed. She was asystole with cool, cyanotic skin. No shock advised on the first responders' defibrillator. I intubated her, did a round of epi down the tube, then got an IV and did 25 minutes of ACLS, including 25 grams of Dextrose because her sugar was less than 20, but got nothing back, and so I presumed her. It wasn't until I came back to the base and was writing up the presumption that I recognized the medical history as someone who I had transported a few days earlier for a broken knee. Dead people really have nothing in their faces because I had not a clue that I had actually been talking to this person so recently.
When I did the tube, I didn't initially see the chords, but with my right hand, I applied crick pressure for myself, using my fingers like the fingers on a flute to find the right spot -- a modification of a technique I learned in a half-day airway class at the JEMS conference in Phillidelphia three years ago. The idea is that the intubator has much better control of the manipulation than a third party. When I pressed down with my middle finger tip the chords dropped right down into view. I said to my partner. "See where I am pressing with my finger. Put your fingertip right there." She put it right in the right spot, and I easily slipped the tube in. The technique doesn't always work so well, but it has helped me out a number of times.
The half-day airway class I took in Philidelphia was taught by Richard M. Levitan, M.D. He is the guy behind the airway cam videos and book. It was a great course. I went to his web site recently and see he offers a two day class with everyone getting their own cadaver for the second day. It's pricey, but I'm thinking about doing it at some point. Anything to help improve my airway skills.
Practical Emergency Airway management Course
Airway Cam Home
Airway Tips
The Airway Cam Guide to Intubation and Practical Emergency Airway Management
A couple years ago, I also took a two day class taught locally called D.A.M.S. (Difficult Airway Management in the Streets) that was also excellent. That was taught by Daniel and David Tauber. The class culminated in an airway tunnel where we had to crawl under tables in a dark room illuminated only by light sticks from one airway station to the next -- each station (there were 10 of them) involved a different airway scenario (basic ET, nasal, broken equipment, pedi, combitube, awkward positining requiring "icepick" technique, etc.)
I have also heard of an airway class called SLAM(Street Level Airway Management) that I would love to take someday.
SLAM
You can never know too much about the airway.
When I did the tube, I didn't initially see the chords, but with my right hand, I applied crick pressure for myself, using my fingers like the fingers on a flute to find the right spot -- a modification of a technique I learned in a half-day airway class at the JEMS conference in Phillidelphia three years ago. The idea is that the intubator has much better control of the manipulation than a third party. When I pressed down with my middle finger tip the chords dropped right down into view. I said to my partner. "See where I am pressing with my finger. Put your fingertip right there." She put it right in the right spot, and I easily slipped the tube in. The technique doesn't always work so well, but it has helped me out a number of times.
The half-day airway class I took in Philidelphia was taught by Richard M. Levitan, M.D. He is the guy behind the airway cam videos and book. It was a great course. I went to his web site recently and see he offers a two day class with everyone getting their own cadaver for the second day. It's pricey, but I'm thinking about doing it at some point. Anything to help improve my airway skills.
Practical Emergency Airway management Course
Airway Cam Home
Airway Tips
The Airway Cam Guide to Intubation and Practical Emergency Airway Management
A couple years ago, I also took a two day class taught locally called D.A.M.S. (Difficult Airway Management in the Streets) that was also excellent. That was taught by Daniel and David Tauber. The class culminated in an airway tunnel where we had to crawl under tables in a dark room illuminated only by light sticks from one airway station to the next -- each station (there were 10 of them) involved a different airway scenario (basic ET, nasal, broken equipment, pedi, combitube, awkward positining requiring "icepick" technique, etc.)
I have also heard of an airway class called SLAM(Street Level Airway Management) that I would love to take someday.
SLAM
You can never know too much about the airway.
Thursday, November 17, 2005
Nursing Home Artwork
I’m wheeling a patient down the hall in nursing home (bringing them back from a dialysis trip), looking at the paintings on the wall. Most nursing homes have really crappy art work -- paintings of rich people having picnics in top hats or girls in nightgowns playing with kittens -- paintings that are sold in crappy five and dime stores for $15 each -- really bland paintings that are supposed to I guess in some way provide comfort and peace and thus cause patients to fall asleep with their mouths open because the paintings are so lifeless and boring. That would be my idea of hell, ending up having to spend my last years looking at those paintings. Please let me out of here!
But this nursing home has a Van Gogh – Irises.
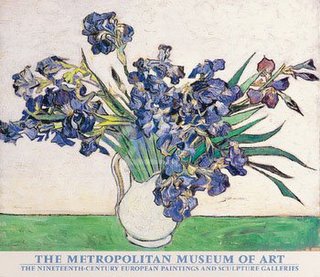
A nice painting.
I could handle a nursing home with a good collection of impressionist prints. I think if I could have any one painting I would want Renoir's Dance at Bougival.
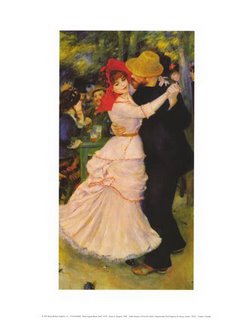
I could stare at that painting and remember what it was like to hold a woman in my arms.
Though I suppose when I am in a nursing home I may be a little demented, and want something that mirrors my inner thoughts. I could ask for a print of Munch’s The Scream:
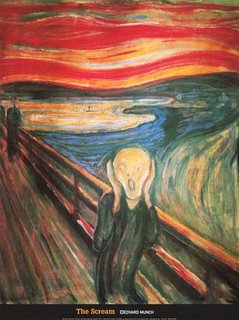
Or some Goya. "Satan Devouring one of His Own Children."
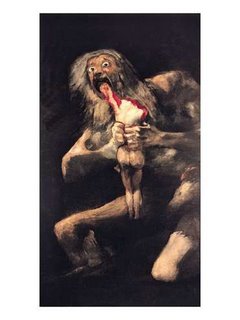
But the administrators probably wouldn't let me hang those up. Can't scare away families looking to place their loved ones.
But this nursing home has a Van Gogh – Irises.
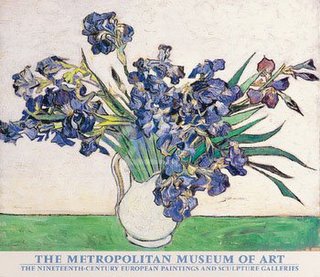
A nice painting.
I could handle a nursing home with a good collection of impressionist prints. I think if I could have any one painting I would want Renoir's Dance at Bougival.
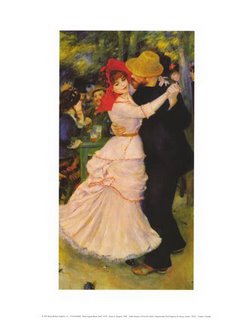
I could stare at that painting and remember what it was like to hold a woman in my arms.
Though I suppose when I am in a nursing home I may be a little demented, and want something that mirrors my inner thoughts. I could ask for a print of Munch’s The Scream:
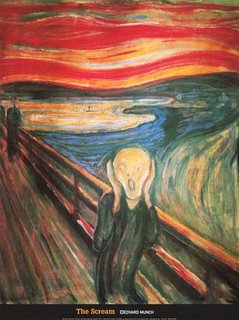
Or some Goya. "Satan Devouring one of His Own Children."
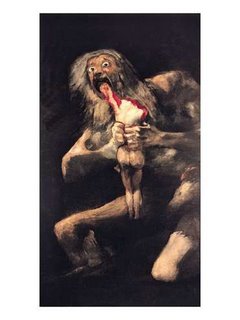
But the administrators probably wouldn't let me hang those up. Can't scare away families looking to place their loved ones.
Sunday, November 13, 2005
EMS Errors/Dangerous Places
Interesting online article at Slate.com about ambulance errors.
Ambulances Can Be Dangerous Places
Here's two excerpts:
In 1999, the Institute of Medicine published its report To Err Is Human, which estimated that up to 98,000 patients may die each year because of the mistakes of doctors, nurses, and other hospital workers. But few published studies have tried to quantify or even characterize the injuries to patients that take place before they reach the hospital. How frequent and how serious are the mistakes that take place in ambulances—and are there simple changes that could help prevent them?
Based on what we know about hospital-based medical error, ambulances may be one of the more dangerous places to be a patient. Studies have shown that medical error is more common when conditions are variable, like in the emergency room, than it is in other parts of the hospital. The problem likely has little to do with experience or skill. Instead it's about the lack of predictability: Doctors and nurses make more mistakes when they work under changing conditions. Think about that and compare the working conditions of paramedics and EMTs with an operating room. Before surgery, an entire staff is prepped with information about a patient's condition, medical history, and the anticipated plan of action. On an ambulance run, there is no plan. Paramedics and EMTs have to improvise as they encounter the obese, frail, terrified, combative, near-dead, stoned, violent, and newly born. And they have to deliver care in a cramped space with relatively few resources.
***
Thought-provoking article, although I would have to disagree with its assumption that ambulances are more dangerous than hospitals. I think in EMS, we have less ways to make errors. In many ways, while our scenes are all varied, the situations are often common -- MI, Stroke, CHF, asthma, hypoglycemia, etc -- and since we have general protocols we follow, the medical care is often routine to us (by routine I don't mean cookbook), even under the most trying circumstances. Difficult situations are after all our norm. Another critical point in our favor is that we are the ones deciding on and providing the care. There are no misunderstandings when one person is both drawing up the drug and delievering it.
***
At my monthly EMS meetings we often talk about the problems of quality assurance. As the number of patient runs increases, and as people charged with QA, whether ambulance service employees or hospital clinical care coordinators have increasing demands on their time, QA inevitably suffers. I recently heard the laments of a fellow paramedic who works for another service complain that his service posted spread sheets detailing employee compliance with filling out billing information -- everything from getting the patient's signature to their next of kin's name -- but nothing has been done to QA the front of the form or discover compliance with taking regular vital signs, giving ASA for chest pain, etc.
***
If there are major errors in EMS, they are most likely system errors. If you were to ask me what is the most dangerous part of being in an ambulance, I would say it is traveling in an ambulance lights and sirens.
Check out this site to view daily ambulance crash logs:
Ambulance Crash Log
Check out these articles from the Detroit News:
Unsafe Saviours
From USA Today:
Speeding to the rescue Can Have Deadly Results
***
For our regional council medical advisory committee, I have been researching lights and sirens protocols to the hospital. Some very interesting items.
1. The National Association of Emergency Medical Services Physicians (NAEMSP) Position Paper on the issue. Use of Warning Lights and Siren in Emergency Medical Vehicle Response and Patient Transport
2. A Merginet Article: Curtailing Emergency Driving Saves Money and Lives
3. A Pennsylvania Regional Council's Newletter Discussing Issue and the new PA regs.Lights and Sirens Use: It is a Big deal to EMS Services!
4: A PA Service's Policy/ Foxwell EMS: (PA): Emergency Response Policy
5. A disccusion group arguing merits/drawbacks of transport AMI patient's lights and sirens. Lights and Sirens Transport of AMI Patients
***
People are just used to lights and sirens being a part of the EMS system even when they are largely unneccessary. This part week they sent us lights and sirens for the 12 year old violent psych, police on scene. The next was also lights and sirens for the 9 year old misbehaving on one of the floors at a pyschiatric hospital. What is wrong with these pictures? Cops on scene and a patient in a psychiatric hospital and they need an ambulance lights and sirens to save the day? In both cases as expected the scenes were well under control before we arrived.
One of the protocols listed above recommends that lights and sirens not be used for cardiac arrests except in cases of trauma, persistent vfib, hypothermia, or drug overdose. I did a code a week ago -- an old woman found face down against the steering wheel of her car outside a doctor's office. She was cold, but still limber. Asystole on the monitor. We worked for a little bit, then since we were already in the ambulance started to the hospital. I told my crew I wanted to go on a priority 2. They revolted. They called me all sorts of names and insisted on going lights and sirens. They said I was crazy. But the lady was dead. Driving fast in fact made CPR harder to do effectively. I am hoping for a sea change in the way we use lights and sirens.
Until there is that sea change, ambulances will continue to be dangerous places.
Ambulances Can Be Dangerous Places
Here's two excerpts:
In 1999, the Institute of Medicine published its report To Err Is Human, which estimated that up to 98,000 patients may die each year because of the mistakes of doctors, nurses, and other hospital workers. But few published studies have tried to quantify or even characterize the injuries to patients that take place before they reach the hospital. How frequent and how serious are the mistakes that take place in ambulances—and are there simple changes that could help prevent them?
Based on what we know about hospital-based medical error, ambulances may be one of the more dangerous places to be a patient. Studies have shown that medical error is more common when conditions are variable, like in the emergency room, than it is in other parts of the hospital. The problem likely has little to do with experience or skill. Instead it's about the lack of predictability: Doctors and nurses make more mistakes when they work under changing conditions. Think about that and compare the working conditions of paramedics and EMTs with an operating room. Before surgery, an entire staff is prepped with information about a patient's condition, medical history, and the anticipated plan of action. On an ambulance run, there is no plan. Paramedics and EMTs have to improvise as they encounter the obese, frail, terrified, combative, near-dead, stoned, violent, and newly born. And they have to deliver care in a cramped space with relatively few resources.
***
Thought-provoking article, although I would have to disagree with its assumption that ambulances are more dangerous than hospitals. I think in EMS, we have less ways to make errors. In many ways, while our scenes are all varied, the situations are often common -- MI, Stroke, CHF, asthma, hypoglycemia, etc -- and since we have general protocols we follow, the medical care is often routine to us (by routine I don't mean cookbook), even under the most trying circumstances. Difficult situations are after all our norm. Another critical point in our favor is that we are the ones deciding on and providing the care. There are no misunderstandings when one person is both drawing up the drug and delievering it.
***
At my monthly EMS meetings we often talk about the problems of quality assurance. As the number of patient runs increases, and as people charged with QA, whether ambulance service employees or hospital clinical care coordinators have increasing demands on their time, QA inevitably suffers. I recently heard the laments of a fellow paramedic who works for another service complain that his service posted spread sheets detailing employee compliance with filling out billing information -- everything from getting the patient's signature to their next of kin's name -- but nothing has been done to QA the front of the form or discover compliance with taking regular vital signs, giving ASA for chest pain, etc.
***
If there are major errors in EMS, they are most likely system errors. If you were to ask me what is the most dangerous part of being in an ambulance, I would say it is traveling in an ambulance lights and sirens.
Check out this site to view daily ambulance crash logs:
Ambulance Crash Log
Check out these articles from the Detroit News:
Unsafe Saviours
From USA Today:
Speeding to the rescue Can Have Deadly Results
***
For our regional council medical advisory committee, I have been researching lights and sirens protocols to the hospital. Some very interesting items.
1. The National Association of Emergency Medical Services Physicians (NAEMSP) Position Paper on the issue. Use of Warning Lights and Siren in Emergency Medical Vehicle Response and Patient Transport
2. A Merginet Article: Curtailing Emergency Driving Saves Money and Lives
3. A Pennsylvania Regional Council's Newletter Discussing Issue and the new PA regs.Lights and Sirens Use: It is a Big deal to EMS Services!
4: A PA Service's Policy/ Foxwell EMS: (PA): Emergency Response Policy
5. A disccusion group arguing merits/drawbacks of transport AMI patient's lights and sirens. Lights and Sirens Transport of AMI Patients
***
People are just used to lights and sirens being a part of the EMS system even when they are largely unneccessary. This part week they sent us lights and sirens for the 12 year old violent psych, police on scene. The next was also lights and sirens for the 9 year old misbehaving on one of the floors at a pyschiatric hospital. What is wrong with these pictures? Cops on scene and a patient in a psychiatric hospital and they need an ambulance lights and sirens to save the day? In both cases as expected the scenes were well under control before we arrived.
One of the protocols listed above recommends that lights and sirens not be used for cardiac arrests except in cases of trauma, persistent vfib, hypothermia, or drug overdose. I did a code a week ago -- an old woman found face down against the steering wheel of her car outside a doctor's office. She was cold, but still limber. Asystole on the monitor. We worked for a little bit, then since we were already in the ambulance started to the hospital. I told my crew I wanted to go on a priority 2. They revolted. They called me all sorts of names and insisted on going lights and sirens. They said I was crazy. But the lady was dead. Driving fast in fact made CPR harder to do effectively. I am hoping for a sea change in the way we use lights and sirens.
Until there is that sea change, ambulances will continue to be dangerous places.
Friday, November 11, 2005
Scouting Report
The local EMT class lets its students sign up to ride with us after they have made it through a certain part of the course. Over the years I have to say most of the students who ride with us don't last. The course has a poor passing rate, and many of the students who do pass rarely enter the field. Every now and then, you get a student that you can glimpse real potential in. There is a young man in the current class I feel this way about.
He comes from a lower middle class family, and was a football player on the state high school championship team a few years ago. He observed with us for the first time last week when we did two calls during the hours he rode. He did well with the blood pressures. If he couldn't hear it, he didn't lie about it. I helped him reposition his stethescope, then he got it properly. We let him pull the stretcher out with the patient on it, and even work the radio with the local CMED. When I explained to him what I was doing, his eyes were fixed on me. I also like that on his own, he made an effort to see that the patient was comfortable, positioning a pillow or pulling up a blanket.
Today was his second time riding. On the first call, he made conversation with the elderly gentleman who had a possible urinary blockage, took his blood pressure and with coaching, gave the radio report to the hospital.
Our second call was for a woman with back pain. She had a history of bulging disks and when she bent down in her office, then straightened up, she did something to her back that was causing her extreme pain. She was in tears when we got there. We tried to get her to sit on the stretcher, but she couldn't manage -- the pain of moving was too great. I called and got orders for morphine. I pushed it slowly, and the woman found the rush very uncomfortable. I stopped at 2 milligrams -- not enough to make a dent in her pain -- she weighed 260. Since we still couldn't get her on the stretcher, I convinced her to let me give her more morphine. I promised to go a little at a time, and very slowly.
The student held her hand while I pushed the medicine through the IV lock. She squeezed his hand tightly. The woman, while in obvious pain, had a great deal of anxiety as well as low tolerance for any procedure -- be it the IV or taking her blood pressure again to make certain her pressure was maintaining. Through it all, the young man, tried to reassure her.
While I was pushing the fifth and sixth milligram -- still unable to get the pain down enough to get her to swing her legs up onto the stretcher, I noticed the young man start to lean. Like a big tree, he slowly teetered, as his eyes rolled back into his head. Then he slumped to the ground. Out cold.
"It's okay," I reassured the patient and the onlookers -- two of her fellow employees. "He just fainted. He'll be okay."
While my partner attended him, I finished giving the woman the morphine.
The young man was helped to a chair, where he hung his head.
"Don't worry," I said, "happens to the best of us."
My partner helped him off with his jacket and outer shirt, then before I knew it, he had resumed his place holding the woman's hand.
"Are you okay?" she asked.
"Yeah," he said. "I just got a little hot. Are you feeling any better?"
"A little," she said, "Thank you."
After ten of morphine and nearly an hour on scene, we finally were on our way to the hospital. The woman, now pain-free, put her hand in his hand. They talked on the way in. At the hospital, he again helped make her comfortable. When he said goodbye, he shook her hand and she wished him well, calling him by his first name.
"Nice job," I said to him as we walked back to the ambulance.
When we got back to the station after the call, he signed up for another shift next week.
I tell you, he can play on my team anytime.
Scouting Report: The kid can take a hit.
He comes from a lower middle class family, and was a football player on the state high school championship team a few years ago. He observed with us for the first time last week when we did two calls during the hours he rode. He did well with the blood pressures. If he couldn't hear it, he didn't lie about it. I helped him reposition his stethescope, then he got it properly. We let him pull the stretcher out with the patient on it, and even work the radio with the local CMED. When I explained to him what I was doing, his eyes were fixed on me. I also like that on his own, he made an effort to see that the patient was comfortable, positioning a pillow or pulling up a blanket.
Today was his second time riding. On the first call, he made conversation with the elderly gentleman who had a possible urinary blockage, took his blood pressure and with coaching, gave the radio report to the hospital.
Our second call was for a woman with back pain. She had a history of bulging disks and when she bent down in her office, then straightened up, she did something to her back that was causing her extreme pain. She was in tears when we got there. We tried to get her to sit on the stretcher, but she couldn't manage -- the pain of moving was too great. I called and got orders for morphine. I pushed it slowly, and the woman found the rush very uncomfortable. I stopped at 2 milligrams -- not enough to make a dent in her pain -- she weighed 260. Since we still couldn't get her on the stretcher, I convinced her to let me give her more morphine. I promised to go a little at a time, and very slowly.
The student held her hand while I pushed the medicine through the IV lock. She squeezed his hand tightly. The woman, while in obvious pain, had a great deal of anxiety as well as low tolerance for any procedure -- be it the IV or taking her blood pressure again to make certain her pressure was maintaining. Through it all, the young man, tried to reassure her.
While I was pushing the fifth and sixth milligram -- still unable to get the pain down enough to get her to swing her legs up onto the stretcher, I noticed the young man start to lean. Like a big tree, he slowly teetered, as his eyes rolled back into his head. Then he slumped to the ground. Out cold.
"It's okay," I reassured the patient and the onlookers -- two of her fellow employees. "He just fainted. He'll be okay."
While my partner attended him, I finished giving the woman the morphine.
The young man was helped to a chair, where he hung his head.
"Don't worry," I said, "happens to the best of us."
My partner helped him off with his jacket and outer shirt, then before I knew it, he had resumed his place holding the woman's hand.
"Are you okay?" she asked.
"Yeah," he said. "I just got a little hot. Are you feeling any better?"
"A little," she said, "Thank you."
After ten of morphine and nearly an hour on scene, we finally were on our way to the hospital. The woman, now pain-free, put her hand in his hand. They talked on the way in. At the hospital, he again helped make her comfortable. When he said goodbye, he shook her hand and she wished him well, calling him by his first name.
"Nice job," I said to him as we walked back to the ambulance.
When we got back to the station after the call, he signed up for another shift next week.
I tell you, he can play on my team anytime.
Scouting Report: The kid can take a hit.
Thursday, November 10, 2005
"You're Going to Need a Bigger Ambulance"
"You're going to need a bigger ambulance," the police officer says when we pull up in our van.
"I don't like the sound of that," my partner says.
Niether do I. Already I can feel my back tightening up.
Inside the small dirty apartment we find a tiny older woman, who points us down a hallway. At the end of the hallway in the bedroom, our patient sits on the edge of his large bed, leaning against a cane. I'm guessing he is 600 pounds -- a wide 600 pounds. The man, in his late thirties, says this is the heaviest he has felt, and his heaviest recorded weight is 619. He says he has been retaining water and feels bloated. "I can't even get up to go to the bathroom anymore," he says. "I had to pee into a water pitcher just now," he says. "Basically I'm drowning in my own fat."
I pride myself on my ability to figure out situations, but when we find out that our bariatric ambulance, which is capable of transporting people up to 1000 pounds is out on a distant call, I am at a loss. Our dispatcher tells us to unscrew our stretcher mount and use a fire department stokes basket. The problem is the local department's basket is only rated for 350 pounds, plus the man cannot lay flat. He is too heavy and too wide to even consider our stretcher. And there is no way he could walk out to the ambulance and try to step in and sit.
While we are trying to figure out what to do, the tiny woman, who by now we know is the patient's mother, asks her son if it is okay if she has a can on his minestone soup. He thinks about it, then says, "okay, I guess, go ahead, you eat it."
Strange.
Back to what to do with him. The only option I see is to get a flatbed truck, but it is pouring rain out. The cop finally comes up with the solution. He looks stable, why don't you just wait for the big ambulance. They tell us it will be an hour and a half at least. But the man's problem is not acute. The bottom line is he's 600 plus pounds and feels crappy because of it. He agrees to wait for the big ambulance, signs a refusal, and says he will call us back if he experiences any problems while waiting.
We go back out to the ambulance and clear. Our dispatcher won't let us leave the scene. He sends a supervisor on a priority to see what is going on. They had sent us on a priority one for difficulty breathing, we have mentioned the patient is large, and now we are clearing refusal. Sounds suspicious, even though we have thoroughly assessed the patient and found him stable and we did set it up with one of the dispatchers to have the big ambulance sent to the address as soon as it is available. We meet the supervisor outside, and explain the situation. This is a chronic problem, not an acute problem. Since we have a bariatric ambulance, and there is no rush, it makes the most sense to wait till it is available, as opposed to taking him in through the rain on the back of a flatbed. He won't fit in one of our van ambulances. The patient prefers to wait for the big ambulance. We go back in to talk to the patient. We find him happily eating cherry popsicles.
***
They station us near the scene. We are certain that when the big ambulance becomes available, we will be sent to do the call. Then we get called for another emergency in the town. While we are on scene, we hear a crew being dispatched for the 600 plus pound man. We hear later that when the crew of the bariatric ambulance takes him in, the hospital staff says, don't leave, he'll be going home as soon as the doctor sees him. Evidently, he is a frequent flyer, although an increasingly larger frequent flyer.
The call we are at is for a man with COPD and a probable respiratory infection. I have taken him in before. He is the man who called the ambulance a few moments before the child was run over by his mother in the same town. If he hadn't called 911 when he did, my partner and I would have been the crew dispatched to that horrific scene. He spared us from that call, and now he has spared us from the 600 pound transport. I shake his hand when I say good bye to him at the hospital.
"I don't like the sound of that," my partner says.
Niether do I. Already I can feel my back tightening up.
Inside the small dirty apartment we find a tiny older woman, who points us down a hallway. At the end of the hallway in the bedroom, our patient sits on the edge of his large bed, leaning against a cane. I'm guessing he is 600 pounds -- a wide 600 pounds. The man, in his late thirties, says this is the heaviest he has felt, and his heaviest recorded weight is 619. He says he has been retaining water and feels bloated. "I can't even get up to go to the bathroom anymore," he says. "I had to pee into a water pitcher just now," he says. "Basically I'm drowning in my own fat."
I pride myself on my ability to figure out situations, but when we find out that our bariatric ambulance, which is capable of transporting people up to 1000 pounds is out on a distant call, I am at a loss. Our dispatcher tells us to unscrew our stretcher mount and use a fire department stokes basket. The problem is the local department's basket is only rated for 350 pounds, plus the man cannot lay flat. He is too heavy and too wide to even consider our stretcher. And there is no way he could walk out to the ambulance and try to step in and sit.
While we are trying to figure out what to do, the tiny woman, who by now we know is the patient's mother, asks her son if it is okay if she has a can on his minestone soup. He thinks about it, then says, "okay, I guess, go ahead, you eat it."
Strange.
Back to what to do with him. The only option I see is to get a flatbed truck, but it is pouring rain out. The cop finally comes up with the solution. He looks stable, why don't you just wait for the big ambulance. They tell us it will be an hour and a half at least. But the man's problem is not acute. The bottom line is he's 600 plus pounds and feels crappy because of it. He agrees to wait for the big ambulance, signs a refusal, and says he will call us back if he experiences any problems while waiting.
We go back out to the ambulance and clear. Our dispatcher won't let us leave the scene. He sends a supervisor on a priority to see what is going on. They had sent us on a priority one for difficulty breathing, we have mentioned the patient is large, and now we are clearing refusal. Sounds suspicious, even though we have thoroughly assessed the patient and found him stable and we did set it up with one of the dispatchers to have the big ambulance sent to the address as soon as it is available. We meet the supervisor outside, and explain the situation. This is a chronic problem, not an acute problem. Since we have a bariatric ambulance, and there is no rush, it makes the most sense to wait till it is available, as opposed to taking him in through the rain on the back of a flatbed. He won't fit in one of our van ambulances. The patient prefers to wait for the big ambulance. We go back in to talk to the patient. We find him happily eating cherry popsicles.
***
They station us near the scene. We are certain that when the big ambulance becomes available, we will be sent to do the call. Then we get called for another emergency in the town. While we are on scene, we hear a crew being dispatched for the 600 plus pound man. We hear later that when the crew of the bariatric ambulance takes him in, the hospital staff says, don't leave, he'll be going home as soon as the doctor sees him. Evidently, he is a frequent flyer, although an increasingly larger frequent flyer.
The call we are at is for a man with COPD and a probable respiratory infection. I have taken him in before. He is the man who called the ambulance a few moments before the child was run over by his mother in the same town. If he hadn't called 911 when he did, my partner and I would have been the crew dispatched to that horrific scene. He spared us from that call, and now he has spared us from the 600 pound transport. I shake his hand when I say good bye to him at the hospital.
Wednesday, November 02, 2005
"For the Unconscious"
Calls run in random, almost crazy patterns that sometimes give you cluster days where you are bombarded with all similar calls. Some days its psychs, other days its carry-downs. (What really sucks is when a carry-down cluster intersects with a humongous patient cluster.) Other days it is asthmas or strokes or MVAs. I once had a cluster month of cardiac arrests where I did 10 in just 12 days of work.
Today was “unconscious” cluster day with a side helping of “cardiac arrest.”
Sign on in the morning and we are sent on a non-priority for a sick person in the north end. While enroute, we are switched to a priority one "for the unconscious" at the train station. Get there and can find no one so we clear no patient. Later we are sent "for the unconscious" also in the north end, possible drug overdose and no one is there. In the afternoon, we are sent "for the unconscious" in the height of rush hour. Arrive to find a man slumped over at a bus stop. He is just drunk.
Earlier we are sent for a “fall possible unconscious” at a chicken restaurant in another town. We find a man lying on the ground writing in pain. He says his knee hurts. He has fallen earlier in the day at a senior center – the man is 90 – he felt okay, then went about his way. While eating chicken, the pain became so unbearable he thought he was going to pass out. His knee looks a little deformed, but then so does his other knee. Only a little pain on palpation. His pressure is 93/60 – he says he usually has low pressure. He says he feels dizzy like he is going to pass out. We take him to the hospital – it is very odd – he looks terrible, but he says the pain in his knee isn’t as bad. The one problem with the call for me is he is hard of hearing and he has the most foul breath – it is so foul – it makes me think there is something wrong with his insides. I have to lean forward to shout at him, but then he answers before I can pull my head away and I get hit with a toxic plume of breath. Very unpleasant. We finally get him in the room at the hospital, and then he starts to puke. He fills up three emesis basins with thick food like emesis.
I am writing up my run form, when I hear on the radio of one of our fly car medics in a suburban town that there was a “cardiac arrest” there. Both fly medics are at the hospital writing their run forms up. I get a page then asking any available car to clear, so my partner and I clear and are sent to the cardiac arrest.
It turns out it isn’t a cardiac arrest, but still an interesting call. A forty year old woman, who has had a cardiac arrest a couple months ago and has an implanted defibrillator was mowing the lawn when the thing went off, knocking her on her back. It went off three more times. She is extremely anxious when we get there and worried she is about to die. It is the first time it has ever gone off. I do what I can to reassure her, as well as giving her some Versed to ease her anxiety and take away some of the pain should the defib go off again. Her kids who were with her when it went off are all bawling and we haveto try to calm them down as well.
Toward the end of the day we are sent "for the unconscious" man in a car. Enroute we get an update from one of the fly car medics that the man is in his car in the garage with the engine running. Then before we can get there we get cancelled. I am guessing the fire department got the man out of the garage and the medic called him dead.
Not two minutes go by before we are sent "for the unconscious" – a woman in a car outside a medical building. We arrive first and a woman directs us to a car where I can see someone sitting in the front seat. “I knocked on the glass,” the woman says, “but she wouldn’t move.” The door is open. The woman in the car is elderly, head slumped forward. She is cool and not breathing, but still limber. I shout to my partner that it is a code, and then I pull her out onto the board and do CPR as we wheel her to the stretcher. One of our supervisors has arrived and then the fly car medic. She is asystole. It is nice having two medics with me. All I have to do is hold out my hand and they hand me the ET tube or drawn up drugs. She has the tiniest chords. I am just barely able to get a 7.0 through them. We transport her to a local hospital, but we don’t get anything back. If she had died at home I would have worked her twenty minutes, then called her, but here the twenty minutes aren’t up until we are reaching the hospital. The doctor in room one calls her dead shortly after hearing our report.
***
One funny or not so funny from the day is when we arrive at the scene of the drunk at the bus stop. We pull in to the bus stop opposite traffic so only my partner can see the patient. I get out the passenger door, grab the blue bag from the side of the ambulance, then go around the back, thinking my partner has gone directly to the patient. As Iwalk around the rear, the back door swings hard right into me, catching me dead on. My partner is pulling out the stretcher and whether it’s him throwing the door open or a fierce gust of wind, the door catches me hard and quite by surprise. I give him a tough time about it. Fortunately at six eight, two-twenty-five, and the fact that I had my arm in front of me holding the strap of the blue bag slung over my shoulder, I avoided being knocked flat onto the pavement. I suppose then my partner would have had to have requested another ambulance "for the unconscious.”
Today was “unconscious” cluster day with a side helping of “cardiac arrest.”
Sign on in the morning and we are sent on a non-priority for a sick person in the north end. While enroute, we are switched to a priority one "for the unconscious" at the train station. Get there and can find no one so we clear no patient. Later we are sent "for the unconscious" also in the north end, possible drug overdose and no one is there. In the afternoon, we are sent "for the unconscious" in the height of rush hour. Arrive to find a man slumped over at a bus stop. He is just drunk.
Earlier we are sent for a “fall possible unconscious” at a chicken restaurant in another town. We find a man lying on the ground writing in pain. He says his knee hurts. He has fallen earlier in the day at a senior center – the man is 90 – he felt okay, then went about his way. While eating chicken, the pain became so unbearable he thought he was going to pass out. His knee looks a little deformed, but then so does his other knee. Only a little pain on palpation. His pressure is 93/60 – he says he usually has low pressure. He says he feels dizzy like he is going to pass out. We take him to the hospital – it is very odd – he looks terrible, but he says the pain in his knee isn’t as bad. The one problem with the call for me is he is hard of hearing and he has the most foul breath – it is so foul – it makes me think there is something wrong with his insides. I have to lean forward to shout at him, but then he answers before I can pull my head away and I get hit with a toxic plume of breath. Very unpleasant. We finally get him in the room at the hospital, and then he starts to puke. He fills up three emesis basins with thick food like emesis.
I am writing up my run form, when I hear on the radio of one of our fly car medics in a suburban town that there was a “cardiac arrest” there. Both fly medics are at the hospital writing their run forms up. I get a page then asking any available car to clear, so my partner and I clear and are sent to the cardiac arrest.
It turns out it isn’t a cardiac arrest, but still an interesting call. A forty year old woman, who has had a cardiac arrest a couple months ago and has an implanted defibrillator was mowing the lawn when the thing went off, knocking her on her back. It went off three more times. She is extremely anxious when we get there and worried she is about to die. It is the first time it has ever gone off. I do what I can to reassure her, as well as giving her some Versed to ease her anxiety and take away some of the pain should the defib go off again. Her kids who were with her when it went off are all bawling and we haveto try to calm them down as well.
Toward the end of the day we are sent "for the unconscious" man in a car. Enroute we get an update from one of the fly car medics that the man is in his car in the garage with the engine running. Then before we can get there we get cancelled. I am guessing the fire department got the man out of the garage and the medic called him dead.
Not two minutes go by before we are sent "for the unconscious" – a woman in a car outside a medical building. We arrive first and a woman directs us to a car where I can see someone sitting in the front seat. “I knocked on the glass,” the woman says, “but she wouldn’t move.” The door is open. The woman in the car is elderly, head slumped forward. She is cool and not breathing, but still limber. I shout to my partner that it is a code, and then I pull her out onto the board and do CPR as we wheel her to the stretcher. One of our supervisors has arrived and then the fly car medic. She is asystole. It is nice having two medics with me. All I have to do is hold out my hand and they hand me the ET tube or drawn up drugs. She has the tiniest chords. I am just barely able to get a 7.0 through them. We transport her to a local hospital, but we don’t get anything back. If she had died at home I would have worked her twenty minutes, then called her, but here the twenty minutes aren’t up until we are reaching the hospital. The doctor in room one calls her dead shortly after hearing our report.
***
One funny or not so funny from the day is when we arrive at the scene of the drunk at the bus stop. We pull in to the bus stop opposite traffic so only my partner can see the patient. I get out the passenger door, grab the blue bag from the side of the ambulance, then go around the back, thinking my partner has gone directly to the patient. As Iwalk around the rear, the back door swings hard right into me, catching me dead on. My partner is pulling out the stretcher and whether it’s him throwing the door open or a fierce gust of wind, the door catches me hard and quite by surprise. I give him a tough time about it. Fortunately at six eight, two-twenty-five, and the fact that I had my arm in front of me holding the strap of the blue bag slung over my shoulder, I avoided being knocked flat onto the pavement. I suppose then my partner would have had to have requested another ambulance "for the unconscious.”
Tuesday, November 01, 2005
Cigarettes and Tasers
We get sent to a nursing home for a “violent” patient in the lobby. Cops have been notified. We arrive to find a big muscular man about fifty with no legs in a motorized wheelchair waving his fist at a nurse, who stands back about ten feet, shaking her head at him. There are three police officers in the room
Here’s the deal. He goes outside to smoke. Sometimes he ventures too far in his chair they are worried he is going to get hit by a car in the parking lot. Plus, his guardian doesn’t want him smoking so for his health they have put an electronic guard on his chair so when he approaches the front door it locks so he can’t get out. For him at least it’s about freedom and his cigarettes. Don’t mess with a man with no legs’s cigarettes.
The cops tell him since he threatened the nurse and threatened himself, or at least said his life wasn’t worth living, he has to go to the hospital for evaluation.
“Take me to jail,” he says.
The cops don’t want to take him to jail. They want him to go with us. He has called their bluff.
“I ain’t going,” he says. "I have rights."
“You’re not going to win this argument,” one of the cops says. “There are five of us and one of you.”
“I ain’t going.”
“I’ve got a taser,” the cop says.
I’m about to suggest that I have Ativan and Haldol and maybe the chemical restraint will be a better idea if he is going to try to resist, but I can see the man is staring at the cop’s holster that holds the taser. He is probably picturing the same scene that I am. The cop tasering the guy. His big body becoming rigid as the electricity shoots through him, then collapsing limply. Maybe even causing him to pee his pants.
“All right,” he says, clearly unhappy. “You going to see my chair gets put in my room?”
“We’ll take care of it,” the cop says.
“They’re a bunch of thieves here,” he says.
“We’ll keep it safe.”
“Fucking assholes won’t let me smoke,” he says as we head out to the ambulance.
**
Postscript 11/14/05
I go back to this nursing home a couple weeks later and find the same man sitting in his wheelchair about thirty feet from the main door. He's just sitting there staring at it, watching it open as people come in, then close again. If he moves forward the door will lock. If he stays where he is, at least he can feel some breeze on his face. I am tempted to tell my partner to hold the door open, then get behind the guy and make a run for it. Nursing home break! I feel really sorry for the guy. On my way out, he is still there. I stop at the rest room in the hall, but the door is locked. "You need to get a key at the desk," he says, helpfully.
Here’s the deal. He goes outside to smoke. Sometimes he ventures too far in his chair they are worried he is going to get hit by a car in the parking lot. Plus, his guardian doesn’t want him smoking so for his health they have put an electronic guard on his chair so when he approaches the front door it locks so he can’t get out. For him at least it’s about freedom and his cigarettes. Don’t mess with a man with no legs’s cigarettes.
The cops tell him since he threatened the nurse and threatened himself, or at least said his life wasn’t worth living, he has to go to the hospital for evaluation.
“Take me to jail,” he says.
The cops don’t want to take him to jail. They want him to go with us. He has called their bluff.
“I ain’t going,” he says. "I have rights."
“You’re not going to win this argument,” one of the cops says. “There are five of us and one of you.”
“I ain’t going.”
“I’ve got a taser,” the cop says.
I’m about to suggest that I have Ativan and Haldol and maybe the chemical restraint will be a better idea if he is going to try to resist, but I can see the man is staring at the cop’s holster that holds the taser. He is probably picturing the same scene that I am. The cop tasering the guy. His big body becoming rigid as the electricity shoots through him, then collapsing limply. Maybe even causing him to pee his pants.
“All right,” he says, clearly unhappy. “You going to see my chair gets put in my room?”
“We’ll take care of it,” the cop says.
“They’re a bunch of thieves here,” he says.
“We’ll keep it safe.”
“Fucking assholes won’t let me smoke,” he says as we head out to the ambulance.
**
Postscript 11/14/05
I go back to this nursing home a couple weeks later and find the same man sitting in his wheelchair about thirty feet from the main door. He's just sitting there staring at it, watching it open as people come in, then close again. If he moves forward the door will lock. If he stays where he is, at least he can feel some breeze on his face. I am tempted to tell my partner to hold the door open, then get behind the guy and make a run for it. Nursing home break! I feel really sorry for the guy. On my way out, he is still there. I stop at the rest room in the hall, but the door is locked. "You need to get a key at the desk," he says, helpfully.
Monday, October 31, 2005
One of the First
Last call of the day is a nursing home transfer. Guy has one leg and sores all over his body. He says he is a former EMT in the city – one of the first.
Friday, October 28, 2005
Power Outage
Several hours earlier a car wiped out a telephone pole, bisecting it, and blowing out the powerlines exploding transformers all the way down the street, leaving half the town without power.
It is still dark when we get called for a lift assist. An old man in a wheelchair meets us at the door with a powerful flashlight in his hand. "She's in here," he says, turning and wheeling into the living room as we follow. There in the dark with just the flashlight now shinning on her face, we see an elderly woman in a big lounge chair with her feet elevated. "I'm stuck," she says. She holds the motorized switch and show us nothing happens when she pushes it. "The electricity is out."
"She needs help getting out. I can't help her," the man in the wheelchair says.
"I have to go to the bathroom," the woman adds. "I can't wait any longer."
We lift her out, and get her standing up against her walker. "Excuse me," she says, making a slow but direct line for the bathroom.
You think about all the people stranded in elevators when the power goes out, but you never think about all the old people stuck with their feet up in their electric lounge chairs.
When she comes back from the bathroom, we help her get set in a smaller chair.
"My heroes," she says. "Thank you, gentlemen."
It is still dark when we get called for a lift assist. An old man in a wheelchair meets us at the door with a powerful flashlight in his hand. "She's in here," he says, turning and wheeling into the living room as we follow. There in the dark with just the flashlight now shinning on her face, we see an elderly woman in a big lounge chair with her feet elevated. "I'm stuck," she says. She holds the motorized switch and show us nothing happens when she pushes it. "The electricity is out."
"She needs help getting out. I can't help her," the man in the wheelchair says.
"I have to go to the bathroom," the woman adds. "I can't wait any longer."
We lift her out, and get her standing up against her walker. "Excuse me," she says, making a slow but direct line for the bathroom.
You think about all the people stranded in elevators when the power goes out, but you never think about all the old people stuck with their feet up in their electric lounge chairs.
When she comes back from the bathroom, we help her get set in a smaller chair.
"My heroes," she says. "Thank you, gentlemen."
Saturday, October 22, 2005
I'll Be at Your Side
What I like best about this job are the moments you observe between people, moments that show the bonds that life creates, that show the love in people's hearts, particuarly the love of a parent for a child.
***
We are sent for a two year old who has fallen through a glass table and is bleeding severely. We get there and the fire department has already wrapped it. They say it is a good sized gash. The boy is in his mother's arms and is wailing away. The bleeding appears to have stopped. We transport the mother, boy and his three year old brother. The mother is Indian. She holds the crying boy, and she says, "Numba two baby, you give me so much trouble, but don't worry, mother loves numba two baby, no matter what trouble you give me. " And she kisses him. I watch as she smiles, admiring her screaming child.
***
We are sent for a violent psych, who turns out to be a ten-year old boy who has taken a golf club to a stop sign, then chased several of his neighbors with the now broken shaft. When we arrive he is in the back of a police car. His mother stands by the open backseat door, talking to the police officer about how they can't get the boy's medications right, while looking with concern at her son. I introduce myself to her, then she in turn, introduces me to her son. The boy is crying, sniffling. I ask him how he's doing. "I'd rather not talk about it," he says. "He's had a hard day," his mother says. I can see the sadness and tiredness in her eyes, but there is no anger there, no hint of a breaking point.
***
We are sent for an overdose. It's not an overdose, but a mother who wants her son to get clean. He's been smoking angel dust and acting like a fool," she says. The man has a big smile as he watches his hands move slowly in front of his eyes. Stoned. As we lead him out of the house, his mother kisses him and said, "I love you, you stupid cabron, you come back here like this again, I'll kill you." She squeezes his hand as he goes by.
***
These moments all happened in the last week -- small moments -- that if you didn't look for them you might not see them at all.
***
When I get home one night this week I find in the mail a bootleg CD I bought at EBay of the Springsteen Hartford Concert. I set it on the CD player and listen to it as I lay in bed after I turn out the light. The sound quality is excellent. I am struck by the lyrics to "Jesus Was an Only Son."
Jesus was an only son
As he walked up Calvary Hill
His mother Mary walking beside him
In the path where his blood spilled
Jesus was an only son
In the hills of Nazareth
As he lay reading the Psalms of David
At his mother's feet
A mother prays, "Sleep tight, my child, sleep well
For I'll be at your side
That no shadow, no darkness, no tolling bell,
Shall pierce your dreams this night"
In the garden at Gethsemane
He prayed for the life he'd never live,
He beseeched his Heavenly Father to remove
The cup of death from his lips
Now there's a loss that can never be replaced,
A destination that can never be reached
A light you'll never find in another's face,
A sea whose distance cannot be breached
Well Jesus kissed his mother's hands
Whispered, "Mother, still your tears,
For remember the soul of the universe
Willed a world and it appeared."
***
I am not a religious man. I believe that when you are dead you are dead. I want to be as good a person as I can be while I am here. Not that I am, but I want to always try.
Sometimes our patients can help show us the way.
***
Years ago I read a great short story by Andre Dubus called "A Father's Story." It is about a priest who finds out his daughter has killed a man in a hit and run accident, and when the police come late in the story and ask him if he knows anything, in anguish, he lies to them. The story ends where he talks to God, and he tells God if it had been one of his sons, he could have turned him in because his sons are strong and he could bear watching them suffer, but his daughter... He asks God if Jesus was God's daughter rather than his son, would he have been able to send her to her death. Very powerful story. A story about a parent's limitless love.
Andre Dubus: Selected Stories
***
We are sent for a two year old who has fallen through a glass table and is bleeding severely. We get there and the fire department has already wrapped it. They say it is a good sized gash. The boy is in his mother's arms and is wailing away. The bleeding appears to have stopped. We transport the mother, boy and his three year old brother. The mother is Indian. She holds the crying boy, and she says, "Numba two baby, you give me so much trouble, but don't worry, mother loves numba two baby, no matter what trouble you give me. " And she kisses him. I watch as she smiles, admiring her screaming child.
***
We are sent for a violent psych, who turns out to be a ten-year old boy who has taken a golf club to a stop sign, then chased several of his neighbors with the now broken shaft. When we arrive he is in the back of a police car. His mother stands by the open backseat door, talking to the police officer about how they can't get the boy's medications right, while looking with concern at her son. I introduce myself to her, then she in turn, introduces me to her son. The boy is crying, sniffling. I ask him how he's doing. "I'd rather not talk about it," he says. "He's had a hard day," his mother says. I can see the sadness and tiredness in her eyes, but there is no anger there, no hint of a breaking point.
***
We are sent for an overdose. It's not an overdose, but a mother who wants her son to get clean. He's been smoking angel dust and acting like a fool," she says. The man has a big smile as he watches his hands move slowly in front of his eyes. Stoned. As we lead him out of the house, his mother kisses him and said, "I love you, you stupid cabron, you come back here like this again, I'll kill you." She squeezes his hand as he goes by.
***
These moments all happened in the last week -- small moments -- that if you didn't look for them you might not see them at all.
***
When I get home one night this week I find in the mail a bootleg CD I bought at EBay of the Springsteen Hartford Concert. I set it on the CD player and listen to it as I lay in bed after I turn out the light. The sound quality is excellent. I am struck by the lyrics to "Jesus Was an Only Son."
Jesus was an only son
As he walked up Calvary Hill
His mother Mary walking beside him
In the path where his blood spilled
Jesus was an only son
In the hills of Nazareth
As he lay reading the Psalms of David
At his mother's feet
A mother prays, "Sleep tight, my child, sleep well
For I'll be at your side
That no shadow, no darkness, no tolling bell,
Shall pierce your dreams this night"
In the garden at Gethsemane
He prayed for the life he'd never live,
He beseeched his Heavenly Father to remove
The cup of death from his lips
Now there's a loss that can never be replaced,
A destination that can never be reached
A light you'll never find in another's face,
A sea whose distance cannot be breached
Well Jesus kissed his mother's hands
Whispered, "Mother, still your tears,
For remember the soul of the universe
Willed a world and it appeared."
-Jesus Was an Only Son
Bruce Springsteen
***
I am not a religious man. I believe that when you are dead you are dead. I want to be as good a person as I can be while I am here. Not that I am, but I want to always try.
Sometimes our patients can help show us the way.
***
Years ago I read a great short story by Andre Dubus called "A Father's Story." It is about a priest who finds out his daughter has killed a man in a hit and run accident, and when the police come late in the story and ask him if he knows anything, in anguish, he lies to them. The story ends where he talks to God, and he tells God if it had been one of his sons, he could have turned him in because his sons are strong and he could bear watching them suffer, but his daughter... He asks God if Jesus was God's daughter rather than his son, would he have been able to send her to her death. Very powerful story. A story about a parent's limitless love.
Andre Dubus: Selected Stories
Thursday, October 20, 2005
Company Man/Union Man
One of my partners used to call me a company man because I used to clear as soon as possible from calls. We'd be in the EMS writing up the run report and the dispatcher would scream. Can anyone clear? I'm holding two calls. Priority One. I'd clear, then she'd bang us with a transfer the company was late on. Fell for it again, he'd say, company man.
I like having pride in my work and my workplace -- not that I always do. The world is not perfect, and the world of EMS even less so. Like everyone I go through periods of agitation about where I work. It is no secret that paramedics and EMTs are among the lowest paid jobs for the work we do, for what is asked of us. That fact has caused many good people to leave the field. Yet here I remain.
***
A couple months ago I was approached by two friends and asked if I could help out with the union contract negotiations. It's ugly this time, one of them said. You won't believe what they are asking us to take.
All my life I have taken on things I shouldn't. I get excited about something then overload myself. Years ago I was asked if I could help out with the fight againt budget cuts at the state EMS office. The next thing I knew I was leading a rally on the capitol (And popping Tums for the first time in my life). Later I was asked to help out with another EMS project and before I knew it I was going to meetings all over the state and serving on several committees, spending all my time writing drafts of proposals. I cut back some on that, but the residual of it is I am on the regional medical and educational committees and am actively involved in projects from rewriting the protocols, designing a protocol exam, and developing a lights and sirens policy.
The one area I have always stayed away from, however, has been getting actively involved in the union. Now, let me say, I am a union man. I believe in unions, I am a proud card carrying union member. I know the words to Joe Hill, as well as many Woody Guthrie songs. But I know that serving on the union is a quagmire that I have not wanted to get stuck in. For years I have watched union leaders get assailed by their fellow employees. It is a thankless job. For no pay and for many hours and days of their time, they get shit from everyone.
I remember calling up one union president and giving him hell years ago because their proposal was going to make me pay more for health insurance because my start date was January 3, where if my start date was December 31 I would be grandfathered in. We almost met in a parking lot to fight it out. Another time I called him up to give him hell about the company forcing me to take a post in the same suburban town where I now work willingly because at the time I was the paramedic with the least seniority of those with the seniority eligible to be posted there and no one else wanted to go(this was back in the day when there were very few medics, transfers for medics were few and far between and we all loved being in the city). He was just trying to do his job, but I didn't like the way he was doing it. Not that he got a dime for it. All the time he was in meetings defending employees, he wasn't getting paid while I was working overtime at time and a half.
Everytime a contract has come up, the union team has been blasted. How come you let them have this provision? How come our wages aren't more? The last contract was terrible. The older employees like me, who had to pay nothing for our health insurance (our one perk that made our low pay palatable), were sold out so the new employees and part-timers would pay less for health insurance. The contract passed on a strict party line vote with the most senior 1/3 voting it down, and everyone else voting for it.)
While I was not happy with the union or the way the union leadership did their job, I could not deny the fact that if instead of spending all their time trying to negotiate a contract or defending no matter how badly their fellow members rights, if they were working as I was instead of doing unpaid union business, all the money they would have gotten would have more than equalled any conceivable munificent raise that might have won through their persistence.
Working for the union means the company hates you, your fellow employees hate you, and you hate yourself because you think you are stupid for even trying to do such a thankless job.
So when they asked me to help out, I told them thanks, but no thanks, I was, ah, busy, yeah(that's the ticket), I was busy with other things. Sorry.
Too busy, working overtime. Too busy making money. Ca-ching.
***
Early word on the contract is not good. The company is trying to shove a new health care plan down our throats. They are offering a pittance for a raise. I have never seen people so upset. The way they are interpreting the health insurance is all it will take is one bad illness in your family and and any savings you have will be wiped out. You'll be bankrupt. A debtor for life. There is no protection at all for catastrophe. I read through the material, and I don't quite see it that way, but when I point out my interpretation, they say, that could be, but the company doesn't have the answers for us. It seems the plan is as confusing to the company negotiators as it is to us. They have promised answers for us, but not delievered. For the first time I hear the "s" word mentioned.
***
Speaking of company men, I know of only one other medic beside me-- there may be more -- who laid down the $2500 a few months back to buy into the company. We own only a measly piece, but we we joke about the "riffraft" in the union who are taking a hardline with the company in the current labor negotiations, trying to eat into our dividends. Nevertheless we the company's initial proposal comes up for a vote, we join with our brothers and sisters (union talk) and vote down the proposal, which is defeated 125-3. In the past, the union has been relatively weak in the face of the company's negotiators, but this year they have formed a stronger front. Pay is pay, but health insurance is a person's family and it illicits a much stronger response. I know health costs are skyrocketing, but people need to be assured that if they get sick or someone in their family is sick, they won't be wiped out.
***
The negotiating resumes and in the first meeting the health insurance questions seem to be getting answered, and people seem to be saying, maybe the plan, which the company has now apparently modified, is not as unreasonable as initially thought. There are many other issues on the table that need to be resolved, but we are hopeful a public confrontation can be avoided. There is nothing wrong with hardball play at contract time -- that's good business (both for the union and the company). In the end I hope both sides can settle on something that works for everyone. While I am a company man, if ever forced to chose, I have to stand on the side of the people who work the streets.
***
Like others I contemplate the worst case scenario. What would I do? I am a union man so that much is clear. I will have to find other work elsewhere. I can start over as a medic at another company if they will hire me, but I will not have the prime suburban shift I have no, nor the ability to work unlimited overtime. How will I be able to meet my mortgage and other obligations? I may have to sell my house.
But it is not that dire. I will be taking an honorable stand, honoring my commitment to my fellow workers, proving the mettle I am made of. And, I think, maybe as one door closes, another may open. Maybe this is what I need to escape the shackles of this job I love. I would now be free to move anywhere in the country. I could go to law school, get a nursing degree, join the Peace Corps, see the world, live in a one room shack somewhere in America and finish my novels and write other, greater ones. Maybe that is what I need. The truth is I am unafraid of the future. What will be will be.
***
While at the hospital I see one of our newer medics. I think she has been a medic maybe 2 or 3 years, after being an EMT for several before that. A nice, smart, well- meaning middle-aged woman -- who cares about being good at her job. She tells me she is going to go part-time (I guess she's going back to her old sales job part-time), and she seems sort of beatup. I don't know whether it is the job, the union negotiations(where she has been actively involved and by many accounts gave an impassioned Norma Rae speech to the company negotiators), or all the routine crap that each profession and workplace has, and which sometimes can be onerous in this one, but she seems tired and disspirited. It makes me sad. You hate to see people who care leave, even if it is just to go part-time.
***
The next negotiating session will be Sunday night. I say I will attend.
***
I'm beat as I have worked the last seven days straight, including twelve hours that day and almost twenty hours the previous day. I am planning to stay for two or three hours at most, just to say I was there. I'm not planning on speaking. I just want to sit in the room.
There are maybe fifteen or sixteen of us, including three people from the union. The management team has six people. They come in the room and give their response to the union's last proposal, then they leave the room, and for the next two hours we talk over all the points. Then we make a counter offer, which we present when they come back in the room, then they leave, we wait and they return with counteroffer. The evening goes like this.
The union members who have been at most of the sessions and who have done the most work are very passionate. I know them well. I used to work with one of the women, another is a good friend. You don't want either of them in your face. Another woman is the closet human to a pit bull I have seen. One of the guys is a long standing medic. I have watched him for years. He is a great medic and a passionate man. I remember one night when he brought in a child whose throat had been slashed -- he intubated the boy by sticking an Et tube right into the boy's open throat. I remembered the pent up rage he let out when he came out of the hospital that night. These are good people -- many with serious illnesses in their immediate families -- cancer, crippling diseases, major operations. I respect all of them.
I would not make a good negotiator. I would come in with a reasonable proposal from the start. Then I would shrug and said okay when I got a counteroffer. If that's the best you can do, I guess we'll have to take it. I don't know if I would have the combination of rage and steel to insist on what I feel I deserve.
I know several of the company team. Nice people. They have their bottom lines too -- their jobs to do.
The people from the union local are also impressive to me. They have been through other negotiations and can offer counsel. They are straight talking and tough. They say they will back us. At the same time they are not offering us pie in the sky versions of reality. The lead union man makes a good point -- the contract we will get is only as strong as we are as a union. We had a good vote, but if it comes to it, will we all stand together?
There is a point when it looks like people are angry and they want to tell the company to shove it. I am reluctant to speak because I have not been there for all the meetings, I have not had to put it out on the line like they have. I haven't had to eat any shit.
I say my peace. I compliment them on what they have achieved -- on their hard work. I respect what they have achieved -- the modifications the company has already made in its proposal in response to their arguements. I tell them that no matter what the outcome, I will stand with. If it means striking, even though it is something I do not want to do, I will strike. But I also tell them, I think the modified contract offer isn't so bad that everyone else will walk on it. When really pressed, I don't know how many will stand with us. Health care is expensive. Its not like all the money is going into the company's coffers. The company is going to be paying 75% of the insurance costs. I agree with what one of my fellow employees has said that if we can get enough to cover the increased cost of the health insurance in the first year, and then a reasonable raise in the next two years, then well, its not such a bad contract all things considered. Are we as a union strong enough to hold our membership together to get what we ought to be paid? (The truth is I don't know if you can make that much). Or should we just look at this as a start. Maybe the next time around, we -- all of us those in the room, and those who are not here -- those working the road, those at home, those who fear losing their jobs and those who don't, can be stronger -- strong enough and committed enough for a tougher battle.
We make what we feel is a reasonable counteroffer. The company comes back with theirs. Some give and take, and by two AM the outline of a deal is reached -- it just needs to be written up. We eat the new health insurance plan (although modified to keep out-of-poket maximims lower than initially offered) and accept a new method of accruing paid time off, along with an attendence policy, but in return we get a decent pay raise and some other extra money for training and longevity.
I am impressed with what I have seen. There was give and take, compromise was made on both sides. Unlike what I have heard about previous meetings, everyone was for the most part civil. I feel a decent contract was agreed upon – a contract which acknowledged the economic times we are in and the rising cost of heath care, and also acknowledged within constraints of the bottom line -- our worth as employees.
So provided our entire membership approves the contract -- there will be no job action and we'll all be working here at least another three years.
I think that is a good thing.
***
I'm at work. I get a page: We need units to clear, holding priority ones. I quickly finish my paperwork (flush), find my partner and tell him we can clear. When we do, they bang us with a transfer.
Company man, I hear my partner say.
***
"There's a better world a-coming
Don't you see, don't you see..."
-Woddy Guthrie
I like having pride in my work and my workplace -- not that I always do. The world is not perfect, and the world of EMS even less so. Like everyone I go through periods of agitation about where I work. It is no secret that paramedics and EMTs are among the lowest paid jobs for the work we do, for what is asked of us. That fact has caused many good people to leave the field. Yet here I remain.
***
A couple months ago I was approached by two friends and asked if I could help out with the union contract negotiations. It's ugly this time, one of them said. You won't believe what they are asking us to take.
All my life I have taken on things I shouldn't. I get excited about something then overload myself. Years ago I was asked if I could help out with the fight againt budget cuts at the state EMS office. The next thing I knew I was leading a rally on the capitol (And popping Tums for the first time in my life). Later I was asked to help out with another EMS project and before I knew it I was going to meetings all over the state and serving on several committees, spending all my time writing drafts of proposals. I cut back some on that, but the residual of it is I am on the regional medical and educational committees and am actively involved in projects from rewriting the protocols, designing a protocol exam, and developing a lights and sirens policy.
The one area I have always stayed away from, however, has been getting actively involved in the union. Now, let me say, I am a union man. I believe in unions, I am a proud card carrying union member. I know the words to Joe Hill, as well as many Woody Guthrie songs. But I know that serving on the union is a quagmire that I have not wanted to get stuck in. For years I have watched union leaders get assailed by their fellow employees. It is a thankless job. For no pay and for many hours and days of their time, they get shit from everyone.
I remember calling up one union president and giving him hell years ago because their proposal was going to make me pay more for health insurance because my start date was January 3, where if my start date was December 31 I would be grandfathered in. We almost met in a parking lot to fight it out. Another time I called him up to give him hell about the company forcing me to take a post in the same suburban town where I now work willingly because at the time I was the paramedic with the least seniority of those with the seniority eligible to be posted there and no one else wanted to go(this was back in the day when there were very few medics, transfers for medics were few and far between and we all loved being in the city). He was just trying to do his job, but I didn't like the way he was doing it. Not that he got a dime for it. All the time he was in meetings defending employees, he wasn't getting paid while I was working overtime at time and a half.
Everytime a contract has come up, the union team has been blasted. How come you let them have this provision? How come our wages aren't more? The last contract was terrible. The older employees like me, who had to pay nothing for our health insurance (our one perk that made our low pay palatable), were sold out so the new employees and part-timers would pay less for health insurance. The contract passed on a strict party line vote with the most senior 1/3 voting it down, and everyone else voting for it.)
While I was not happy with the union or the way the union leadership did their job, I could not deny the fact that if instead of spending all their time trying to negotiate a contract or defending no matter how badly their fellow members rights, if they were working as I was instead of doing unpaid union business, all the money they would have gotten would have more than equalled any conceivable munificent raise that might have won through their persistence.
Working for the union means the company hates you, your fellow employees hate you, and you hate yourself because you think you are stupid for even trying to do such a thankless job.
So when they asked me to help out, I told them thanks, but no thanks, I was, ah, busy, yeah(that's the ticket), I was busy with other things. Sorry.
Too busy, working overtime. Too busy making money. Ca-ching.
***
Early word on the contract is not good. The company is trying to shove a new health care plan down our throats. They are offering a pittance for a raise. I have never seen people so upset. The way they are interpreting the health insurance is all it will take is one bad illness in your family and and any savings you have will be wiped out. You'll be bankrupt. A debtor for life. There is no protection at all for catastrophe. I read through the material, and I don't quite see it that way, but when I point out my interpretation, they say, that could be, but the company doesn't have the answers for us. It seems the plan is as confusing to the company negotiators as it is to us. They have promised answers for us, but not delievered. For the first time I hear the "s" word mentioned.
***
Speaking of company men, I know of only one other medic beside me-- there may be more -- who laid down the $2500 a few months back to buy into the company. We own only a measly piece, but we we joke about the "riffraft" in the union who are taking a hardline with the company in the current labor negotiations, trying to eat into our dividends. Nevertheless we the company's initial proposal comes up for a vote, we join with our brothers and sisters (union talk) and vote down the proposal, which is defeated 125-3. In the past, the union has been relatively weak in the face of the company's negotiators, but this year they have formed a stronger front. Pay is pay, but health insurance is a person's family and it illicits a much stronger response. I know health costs are skyrocketing, but people need to be assured that if they get sick or someone in their family is sick, they won't be wiped out.
***
The negotiating resumes and in the first meeting the health insurance questions seem to be getting answered, and people seem to be saying, maybe the plan, which the company has now apparently modified, is not as unreasonable as initially thought. There are many other issues on the table that need to be resolved, but we are hopeful a public confrontation can be avoided. There is nothing wrong with hardball play at contract time -- that's good business (both for the union and the company). In the end I hope both sides can settle on something that works for everyone. While I am a company man, if ever forced to chose, I have to stand on the side of the people who work the streets.
***
Like others I contemplate the worst case scenario. What would I do? I am a union man so that much is clear. I will have to find other work elsewhere. I can start over as a medic at another company if they will hire me, but I will not have the prime suburban shift I have no, nor the ability to work unlimited overtime. How will I be able to meet my mortgage and other obligations? I may have to sell my house.
But it is not that dire. I will be taking an honorable stand, honoring my commitment to my fellow workers, proving the mettle I am made of. And, I think, maybe as one door closes, another may open. Maybe this is what I need to escape the shackles of this job I love. I would now be free to move anywhere in the country. I could go to law school, get a nursing degree, join the Peace Corps, see the world, live in a one room shack somewhere in America and finish my novels and write other, greater ones. Maybe that is what I need. The truth is I am unafraid of the future. What will be will be.
***
While at the hospital I see one of our newer medics. I think she has been a medic maybe 2 or 3 years, after being an EMT for several before that. A nice, smart, well- meaning middle-aged woman -- who cares about being good at her job. She tells me she is going to go part-time (I guess she's going back to her old sales job part-time), and she seems sort of beatup. I don't know whether it is the job, the union negotiations(where she has been actively involved and by many accounts gave an impassioned Norma Rae speech to the company negotiators), or all the routine crap that each profession and workplace has, and which sometimes can be onerous in this one, but she seems tired and disspirited. It makes me sad. You hate to see people who care leave, even if it is just to go part-time.
***
The next negotiating session will be Sunday night. I say I will attend.
***
I'm beat as I have worked the last seven days straight, including twelve hours that day and almost twenty hours the previous day. I am planning to stay for two or three hours at most, just to say I was there. I'm not planning on speaking. I just want to sit in the room.
There are maybe fifteen or sixteen of us, including three people from the union. The management team has six people. They come in the room and give their response to the union's last proposal, then they leave the room, and for the next two hours we talk over all the points. Then we make a counter offer, which we present when they come back in the room, then they leave, we wait and they return with counteroffer. The evening goes like this.
The union members who have been at most of the sessions and who have done the most work are very passionate. I know them well. I used to work with one of the women, another is a good friend. You don't want either of them in your face. Another woman is the closet human to a pit bull I have seen. One of the guys is a long standing medic. I have watched him for years. He is a great medic and a passionate man. I remember one night when he brought in a child whose throat had been slashed -- he intubated the boy by sticking an Et tube right into the boy's open throat. I remembered the pent up rage he let out when he came out of the hospital that night. These are good people -- many with serious illnesses in their immediate families -- cancer, crippling diseases, major operations. I respect all of them.
I would not make a good negotiator. I would come in with a reasonable proposal from the start. Then I would shrug and said okay when I got a counteroffer. If that's the best you can do, I guess we'll have to take it. I don't know if I would have the combination of rage and steel to insist on what I feel I deserve.
I know several of the company team. Nice people. They have their bottom lines too -- their jobs to do.
The people from the union local are also impressive to me. They have been through other negotiations and can offer counsel. They are straight talking and tough. They say they will back us. At the same time they are not offering us pie in the sky versions of reality. The lead union man makes a good point -- the contract we will get is only as strong as we are as a union. We had a good vote, but if it comes to it, will we all stand together?
There is a point when it looks like people are angry and they want to tell the company to shove it. I am reluctant to speak because I have not been there for all the meetings, I have not had to put it out on the line like they have. I haven't had to eat any shit.
I say my peace. I compliment them on what they have achieved -- on their hard work. I respect what they have achieved -- the modifications the company has already made in its proposal in response to their arguements. I tell them that no matter what the outcome, I will stand with. If it means striking, even though it is something I do not want to do, I will strike. But I also tell them, I think the modified contract offer isn't so bad that everyone else will walk on it. When really pressed, I don't know how many will stand with us. Health care is expensive. Its not like all the money is going into the company's coffers. The company is going to be paying 75% of the insurance costs. I agree with what one of my fellow employees has said that if we can get enough to cover the increased cost of the health insurance in the first year, and then a reasonable raise in the next two years, then well, its not such a bad contract all things considered. Are we as a union strong enough to hold our membership together to get what we ought to be paid? (The truth is I don't know if you can make that much). Or should we just look at this as a start. Maybe the next time around, we -- all of us those in the room, and those who are not here -- those working the road, those at home, those who fear losing their jobs and those who don't, can be stronger -- strong enough and committed enough for a tougher battle.
We make what we feel is a reasonable counteroffer. The company comes back with theirs. Some give and take, and by two AM the outline of a deal is reached -- it just needs to be written up. We eat the new health insurance plan (although modified to keep out-of-poket maximims lower than initially offered) and accept a new method of accruing paid time off, along with an attendence policy, but in return we get a decent pay raise and some other extra money for training and longevity.
I am impressed with what I have seen. There was give and take, compromise was made on both sides. Unlike what I have heard about previous meetings, everyone was for the most part civil. I feel a decent contract was agreed upon – a contract which acknowledged the economic times we are in and the rising cost of heath care, and also acknowledged within constraints of the bottom line -- our worth as employees.
So provided our entire membership approves the contract -- there will be no job action and we'll all be working here at least another three years.
I think that is a good thing.
***
I'm at work. I get a page: We need units to clear, holding priority ones. I quickly finish my paperwork (flush), find my partner and tell him we can clear. When we do, they bang us with a transfer.
Company man, I hear my partner say.
***
"There's a better world a-coming
Don't you see, don't you see..."
-Woddy Guthrie
Subscribe to:
Posts (Atom)